Vitamin B12
Update On Clinical Applications
Abstract
Vitamin B12 is an essential co-factor for methionine synthase and L-methyl-malonyl-CoA mutase, which are required in DNA synthesis and vital in hematopoietic pathways. There are several risk factors for B12 deficiency and associated anemia, including vegetarian or vegan diets and increasing age. Supplemental vitamin B12 is overwhelmingly safe and although there is insufficient evidence to establish the best long term route of administration for B12, the evidence suggests that oral, intramuscular, and parenteral administration are equally effective. Homocysteine and vitamin B12 levels should be routinely checked in individuals with cognitive decline and Alzheimer’s disease, as vitamin B12 is a viable treatment option. The totality of evidence is unclear as to the independent impact of vitamin B12 in relation to cardiovascular risk, but key studies will be discussed. Vitamin B12 is effective at ameliorating the symptoms of depression, as shown by improvements in various validated questionnaires. This article reviews the trials conducted using supplemental vitamin B12 in the treatment of these various health conditions and provides a clinical update.
Introduction
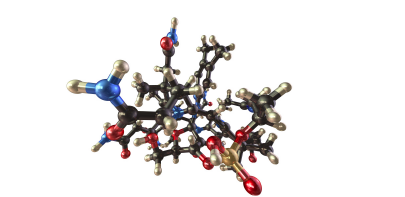
Vitamin B12, also known as cobalamin, can come in many forms including cyano-, methyl-, and hydroxy-cobalamin, among others (O’Leary 2010). It is involved in many physiological pathways in the body and a deficiency causes megaloblastic anemia, as well as a potential host of other damaging consequences. Serum B12 is currently the principle means of assessing B12 status (Carmel 2009), and as discussed below this test alone is insufficient for accurately establishing all stages of B12 deficiency. The addition of holotranscobalamin, methylmelonic acid, and homocysteine to the standard serum B12 measurement provides a more accurate assessment of functional B12 status (Herrmann 2003). Utilizing this expanded four test profile to assess B12 status can help to identify earlier stages of deficiency and initiate appropriate treatment before the manifestation of clinically evident deficiency symptoms (Herrmann 2003). Supplemental vitamin B12 is overwhelmingly safe and no toxic effects have been encountered from administration, indicating that B12 is essentially nontoxic (Food and Nutrition Board 1998). This is applicable when administering amounts at or below the recommended dietary allowance. However, there is limited data for high-dose B12 and there have been some reports of mild side effects such as rash, pruritus, and diarrhea. There is also not enough data to make any conclusions about the safety of large doses of vitamin B12 in pregnancy and breast feeding. In addition to anemia, vitamin B12 has been used as a treatment for numerous health issues, including for cardiovascular health, in depression, and for cognitive health. This article will review the evidence available in each of these areas and update practitioners on the clinical applications of vitamin B12.
Anemia Recent estimates suggest up to 14% of anemias may be associated with folate or vitamin B12 deficiency (Pang 2012). Vitamin B12 is an essential co-factor for methionine synthase and L-methyl-malonyl-CoA mutase, which are required in DNA synthesis and thus vital in hematopoietic pathways (O’Leary 2010). There are several risk factors for B12 deficiency and associated anemia, including vegetarian and vegan diets (Pawlak 2013), and increasing age (Chatthanawaree 2013, Park 2006). An important and often overlooked risk of vitamin B12 deficiency is depletion from drug interactions including proton pump inhibitors, metformin, anti-seizure medications, and nitric oxide (Mazokopakis 2008). Also of interest is a recent study indentifying an increased risk of vitamin B12 (as well as folate and iron) deficiency in patients following gastric bypass, with over 60% developing anemia within three years (Vargas-Ruiz 2008).
The most common anemia associated with vitamin B12 is pernicious anemia (PA), a macrocytic anemia caused by atrophic gastritis and an associated loss of intrinsic factor (IF), which is required to cleave vitamin B12 from protein sources thereby facilitating absorption (Stabler 2013). PA is most common in the seventh or eighth decade of life, with milder atrophic gastritis affecting an estimated 20% of older individuals (Stabler 2013). Long term risk factors of neurologic complications including peripheral neuropathy, and lateral spinal cord and cerebrum lesions, can be prevented or reversed if PA is recognized early in disease progression and supplemental vitamin B12 is provided (Annibale 2011). Since oral supplements provide vitamin B12 unbound to protein even in the absence of IF, absorption can still occur. PA has an insidious onset with non-descript signs and symptoms including fatigue, weakness, headaches, lack of concentration, paresthesias, and digestive disturbance, making it challenging, but important to diagnose early (O’Leary 2010). Patients with PA should be given supplemental doses of at least 500-1000mcg (O’Leary 2010).
Several studies investigating the merits of intramuscular, parenteral, and oral administration routes of vitamin B12 have concluded that in the short term, oral supplementation is equally as effective as other routes in cases of pernicious anemia and malabsoprtion (Seal 2002). Complicating the implications of study results is the common use of the cyanocobalamin form of vitamin B12 (hydroxy, and methyl are available commercially and used clinically), variety in dosing regimens, and unclear long-term comparisons of administration routes. Although cost of oral supplementation is significantly less than IM or parenteral, both IM and parenteral may be more effective in cases where compliance is an issue (Drug and Therapeutics Bulletin 2009).
Establishing parameters to measure B12 deficiency is not straightforward. Traditionally the lower limit of reference ranges for serum B12 reflected the level at which megaloblastic anemia normally presented (O’Leary 2010). While serum testing of total vitamin B12 is available and regularly used, it may misrepresent vitamin B12 status as it includes B12 in the form of hepatocorrin, which is biologically unavailable (Green 2011). More recently holotranscobolamin II, the available form of vitamin B12, has been recognized as a useful measure of B12 status (Green 2011). Measurements of other metabolic markers of vitamin B12 status are helpful in determining not only vitamin B12 status, but also differentiating vitamin B12 and folate deficiencies. Elevated levels of both homocysteine and methylmalonic acid are regularly noted in B12 deficiency, while homocysteine elevation with normal methylmalonic acid levels are more common in folate deficiency, although both markers may be elevated with normal B12 and folate status (Green 2011). Vitamin B12 deficiency is a risk factor for anemia and routine screening of haematological markers along with serum vitamin B12, homocysteine, and methylmalonic acid should be evaluated in individuals at risk of B12 deficiency, specifically elderly and vegetarian populations. Additionally, appropriate identification of PA is crucial in preventing serious long-term consequences. There is insufficient evidence to establish the best long term route of administration for B12, although oral, intramuscular, and parenteral administration appear to be equivocal in the short-term.
Cardiovascular Health Many prospective intervention studies have examined the role of vitamin B12 in cardiovascular disease. Unfortunately, there have been a number of limitations to these trials, including inadequate treatment with vitamin B12 and confounding effects from other simultaneous treatments (Righetti 2009). One recent systematic review of cohort studies included seven studies with varying populations, length of follow-up, study outcomes, and data analysis (Rafnsson 2011). Only one high-quality study reported that low B12 increased the risk of incident cerebral ischaemia. After controlling for homocysteine, the association persisted although weakened, suggesting that the effects of low B12 were only partly mediated by homocysteine. In two studies, higher B12 levels were associated with a greater risk of total mortality and combined fatal and non-fatal coronary events (Rafnsson 2011).
In examining other trials that were excluded from the aforementioned systematic review, there are two that stand out. The first is the Vitamin Intervention for Stroke Prevention Trial (Spence 2007). In the original interpretation of the trial, it was shown that vitamin therapy (B12, B6, folate) had no benefit for homocysteine lowering. However, there were problems with the trial, including the lack of a placebo control, the use of a multiple vitamin with low doses of vitamins, patients in both arms of the trial received injections of B12, and folate fortification of grain products in North America coincided with the initiation of the trial. Upon further interpretation of a subgroup from which patients who could not have responded to the study treatment were excluded, there was a significant reduction of stroke, coronary events, and death. When stratified by median entry level of B12, serum B12 status was the key determinant of response, with those with high serum B12 at entry who received high-dose vitamin (0.4mg cyano-cobalamin was considered the high-dose) had a 33% reduction of events compared to those with low B12 who received low-dose vitamins (Spence 2007). The second trial of interest is the Heart Outcomes Prevention Evaluation 2 Trial (Lonn 2006). In this trial, they evaluated whether long-term therapy with folic acid 2.5mg and vitamins B6 50mg and B12 1mg reduced the risk of major cardiovascular events in a high-risk population. The results showed a 25% significant reduction of stroke with vitamin therapy (p = 0.03), but the authors considered this a chance finding (Lonn 2006). Overall, the totality of evidence is unclear as to the independent impact of vitamin B12 in relation to cardiovascular risk. It is also difficult to make large generalizations based on studies with a range of doses, with limited experimental evidence available for supplemental doses above 1mg of B12.
Depression Low levels of vitamin B12 have been measured in patients with depressive disorders and in some studies, women with metabolically significant deficiencies have been found to have a two-fold higher risk of depression (Penninx 2000). Although many studies examine both folate and vitamin B12, one study has suggested B12 deficiency is independently related to depressive disorders (Tiemeier 2002). A separate study conducted with outpatients diagnosed with major depressive disorder looked at vitamin B12 levels and the consequent six-month treatment outcomes (Hintikka 2003). The authors examined haematological indices, including erythrocyte folate and serum vitamin B12 levels. The study included 115 outpatients with DSM-III-R major depressive disorder at baseline. The 17-item Hamilton Depression Rating Scale was compiled. The results showed that higher vitamin B12 levels were significantly associated with a better outcome at six-months (Hintikka 2003). More recently, a Finnish population-based study examined the association between vitamin B12 levels and melancholic depressive symptoms (Seppala 2013). Subjects were randomly selected from the National Population Register as part of the Finnish diabetes prevention program and the study consisted of 2806 participants. Health examinations were carried out and depressive symptoms were based on the Beck Depression Inventory. Groups were further divided by melancholic or non-melancholic subgroups based on the DSM-IV. The results showed that the mean vitamin B12 level was associated with melancholic depressive symptoms (Seppala 2013).
Many case studies have reported that supplemental vitamin B12 and folic acid can improve the symptoms of depression (Mitchell 2007). In this study, a sample of 12 outpatients with dysthymic disorder was supplemented with 800mcg of folic acid and 1000mcg of vitamin B12 for six weeks. Two instruments were used to measure depressive symptoms: the Beck Depression Inventory- II and the Symptom Checklist-90-Revised. At the end of the six weeks, the raw and t-scores of each of the participants indicated a reduction in the reported levels of symptoms of depression (Mitchell 2007). One large study examined the effects of dietary intake of vitamin B6, folate, and vitamin B12 on depressive symptoms (Skarupski 2010). The study sample consisted of 3503 adults aged over 65 years from the Chicago Health and Aging project. Dietary assessment was made by food-frequency questionnaire and incident depression was measured by the presence of at least four depressive symptoms from the 10-item version of the Center for Epidemiologic Studies Depression scale. The results showed that the higher total intakes of vitamin B6 and B12 were associated with a decreased likelihood of depression for up to 12 years of follow-up, after adjustments were made, including for antidepressant medication use. Each 10 additional milligrams of vitamin B6 and 10 additional micrograms of vitamin B12 were associated with 2% lower odds of depressive symptoms per year (Skarupski 2010). Finally, the B-VITAGE trial is a double-blind, placebo-controlled, randomized trial of homocysteine lowering treatment of depression in later life that is currently in progress (Ford 2010). Participants will receive daily citalopram (20-40mg), plus vitamin B12 (0.4mg), B6 (25mg), and folic acid (2mg) compared to citalopram plus placebo. Over the course of 52 weeks, depressive symptoms will be measured using validated questionnaires. This trial will clarify whether the systematic use of B-vitamins improve the response of older adults to standard antidepressant treatment. Although teasing out the specific effects of vitamin B12 is difficult, the evidence that is available suggests it is both a safe and effective option in the treatment of depressive symptoms.
Cognitive Decline and Alzheimer Disease Vitamin B12 deficiency and elevations in associated biomarkers of low vitamin B12 status, are associated with cognitive decline (CD) (Riggs 1996), including Alzheimer Disease (AD) (Wang 2001). The mechanism implicated in the relationship between Vitamin B12 status and CD is the homocysteine lowering effect of B12 (Werder 2010). Studies have shown that in individuals with elevated homocysteine levels and CD, reducing homocysteine through therapies including combinations of folate, vitamin B12, and vitamin B6, has a favourable benefit on cognitive function (Nilsson 2001).
Results of RCTs evaluating vitamin B12 supplementation as a treatment for CD and AD are mixed (Malouf 2003). Although a number of RCTs are available, due to small sample size and poor study design, a large number do not provide significant power with which to draw conclusions (Malouf 2003). Factors including dose and duration of treatment, extent and duration of cognitive decline, homocysteine levels, vitamin B12 status (and laboratory techniques used for evaluation), all confound results. A 2003 Cochrane review included only two RCTs evaluating vitamin B12 supplementation in the treatment of CD and AD, and concluded insufficient evidence of efficacy, primarily due to small trial size (Malouf 2003). Several newer studies demonstrate positive outcomes with supplemental B12 (0.5mg) in CD, with the largest effect in individuals with elevated homocysteine levels and with the shortest duration of cognitive decline (De Jager 2013). Additionally, studies have demonstrated a decrease in accelerated brain atrophy in both AD (Douaud 2013) and mild CD with homocysteine-lowering therapy by vitamin B12, folate and vitamin B6 (Smith 2010).
Supplemental B12 in combination with folate also shows benefit in as a preventative therapy in decreasing cognitive decline in older individuals with depressive disorders. A 2012 RCT showed significant improvement in cognitive measures after 24 months of supplementation of Vitamin B12 (100mcg) and folate in individuals over 60 (Walker 2012). Of note, in combination therapy with folate, one RCT showed no statistically significant improvement in CD with supplementation, which was likely due to the inclusion of individuals with low or normal homocysteine levels, suggesting lowering homocysteine below normal levels is of no benefit in CD (Pratico 2009). Although there is conflicting evidence represented in research regarding vitamin B12 supplementation in the treatment of CD and AD, there is significant evidence that supplementation in individuals with elevated homocysteine levels early in CD is effective (Walker 2012). Based on the relative safety of vitamin B12 administration and possible degree of benefit, homocysteine and vitamin B12 levels should be routinely checked in individuals with cognitive decline and vitamin B12 (along with folate and vitamin B6) considered as a viable treatment option to lower homocysteine and improve markers of mild CD and AD.
Conclusion
Supplemental vitamin B12 is overwhelmingly safe and no toxic effects have been encountered, especially at doses at or below 1000mcg. Regarding optimal route of administration, there is insufficient evidence to establish the best long term option, but oral, intramuscular, and parenteral administration are all adequate in the short-term. It is imperative to detect vitamin B12 deficiency in those at risk, especially the elderly. Vitamin B12 is an effective treatment for anemia in these cases. Despite some promising results, the totality of evidence is unclear as to the independent impact of vitamin B12 in relation to cardiovascular risk. Vitamin B12 is effective in treating the symptoms of depression, as shown by improvements in various validated questionnaires. Additional well-designed trials are currently in progress. Finally, earlier studies on CD and AD had small sample sizes and poor designs, but newer trials have shown that B12 supplementation in individuals with elevated homocysteine levels early in CD is effective, even in small doses.
References
Annibale B, Lahner E, Fave GD. Diagnosis and Management of Pernicious Anemia. Curr Gastroenterol Rep. 2011;13(6):518–24.
Carmel, R. Mild transcobalamin I (haptocorrin) deficiency and low serum cobalamin
concentrations. Clin Chem. 2003, 49(8):1367-74.
Chatthanawaree W. Biomarkers of cobalamin (vitamin B12) deficiency and its application. J Nutr Health Aging. 2011;15(3):227–31.
De Jager C a, Oulhaj A, Jacoby R, Refsum H, Smith AD. Cognitive and clinical outcomes of homocysteine-lowering B-vitamin treatment in mild cognitive impairment: a randomized controlled trial. Int J Geriatr Psychiatry. 2012;27(6):592–600.
Douaud G, Refsum H, De Jager C a, Jacoby R, Nichols TE, Smith SM, Smith AD. Preventing Alzheimer’s disease-related gray matter atrophy by B-vitamin treatment. Proceedings of the National Academy of Sciences of the United States of America. National Academy of Sciences. 20418; 2013;110(23):9523–8.
Drug and Therapeutics Bulletin. Oral or intramuscular vitamin B 12? DTB BMJ. 2009;47(2):19–21.
Food and Nutrition Board. Dietary reference intakes for thiamin, riboflavin, niacin, vitamin B6, folate, vitamin B12, pantothenic acid, biotin, and choline. Washington, DC: National Academy Press, 1998.
Ford AH, Flicker L, McCaul K, van Bockxmeer F, Hegarty S, Hirani V, Fenner S, Almeida OP. The B-VITAGE trial: a randomized trial of homocysteine lowering treatment of depression in later life. Trials. 2010;11:8
Green R. Indicators for assessing folate and vitamin B 12 status and for monitoring the efficacy of intervention strategies. Am J Clin Nutr. 2011;94(suppl):666S–72S.
Herrmann W, Schorr H, Obeid R, Geisel J. Vitamin B-12 status, particularly holotranscobalamin II and methylmalonic acid concentrations, and hyperhomocysteinemia in vegetarians. Am J clin Nutr 2003;78:131-6
Lonn E, Held C, Arnold JM, Probstfield J, McQueen M, Micks M, Pogue J, Sheridan P, Bosch J, Genest J, Yusuf S, HOPE-2 Investigators. Rationale, design and baseline characteristics of a large, simple, randomized trial of combined folic acid and vitamins B6 and B12 in high risk patients: the Heart Outcomes Prevention Evaluation (HOPE)-2 trial. Can J Cardiol. 2006; 22(1):47-53
Malouf R, Areosa Sastre A. Vitamin B12 for Cognition. Cochrane Database Syst Rev 2003;3.
Mazokopakis EE, Starakis IK. Recommendations for diagnosis and management of metformin-induced vitamin B12 (Cbl) deficiency. Diabetes Res Clin Pr. 2012; 97(3):359–67.
Mitchell JA. The Effect of Folic Acid and B12 on Depression: Twelve Case Studies. J Orthomolecular Med. 2007;22(4):183-192
O’Leary F, Samman S. Vitamin B12 in health and disease. Nutrients. 2010;2(3):299–316.
Nilsson K, Gustafson L, Hultberg B. Improvement of cognitive functions after cobalamin/folate supplementation in elderly patients with dementia and elevated plasma homocysteine. Int J Geriatr Psychiatry. 2001;16(6):609–14.
Pang WW, Schrier SL. Anemia in the elderly. Curr Opin Hematol. 2012;19(3):133–40.
Park S, Johnson MA. What is an Adequate Dose of Oral Vitamin B 12 in Older People with Poor Vitamin B 12 Status? Nutr Rev. 2006;64(8):373–8.
Pawlak R, Parrott SJ, Raj S, Cullum-Dugan D, Lucus D. How prevalent is vitamin B(12) deficiency among vegetarians? Nutr Rev. 2013;71(2):110–7.
Penninx BWJH, Guralink JM, Ferucci L, Fried LP, Allen RH, Stabler SP. Vitamin B12 deficiency and depression in physically disabled older women: Epidemiologic evidence from the women’s health and aging study. Am J Psychiatry. 2000; 157:715-721
Pratico D. High-dose vitamin supplements and Alzheimer disease. JAMA. 2009;301(10):1020–1.
Rafnsson SB, Saravanan P, Bhopal RS, Yajnik CS. Is a low blood level of vitamin B12 a cardiovascular and diabetes risk factor? A systematic review of cohort studies. Eur J Nutr 2011;50:97-106
Righetti M. Protective effect of vitamin B therapy on bone and cardiovascular disease. Recent Pat Cardiovasc Drug Discov. 2009;4(1):37-44
Riggs KM, Spiro A, Tucker K, Rush D. Relations of vitamin B-12 , vitamin B-6, folate, and homocysteine to cognitive performance in the Normative Aging Study. Am J Clin Nutr. 1996;63(3):306–14.
Seal E, Metz J, Flicker L, Melny J. Oral Vitamin B 12 Supplementation in Older Patients with Subnormal or Borderline Serum Vitamin B 12 Concentrations. J Am Geriatr Soc. 2002;50:146–51.
Seppala J, Koponen H, Kautiainen H, Eriksson JG, Kampman O, Leiviska J, Mannisto S, Mantyselka P, Oksa H, Ovaskainen Y, Viikki M, Vanhala M, Seppala J. Association between vitamin b 12 levels and melancholic depressive symptoms: a Finnish population-based study. BMC Psychiatry. 2013;13(1):145.
Skarupski KA, Tagney C, Li H, Ouyang B, Evans DA, Morris MC. Longitudinal association of vitamin B-6, folate, and vitamin B-12 with depressive symptoms among older adults over time. Amer J Clin Nutr. 2010;92(2):330-5
Smith DA, Smith SM, de Jager CA, Whitbread P, Johnston C, Agacinski G, Oulhaj A, Bradley KM, Jacoby R, Refsum H. Homocysteine-lowering by B vitamins slows the rate of accelerated brain atrophy in mild cognitive impairment: a randomized controlled trial. PloS One. 2010;5(9):e12244.
Spence JD. Perspective on the efficacy analysis of the Vitamin Intervention for Stroke Prevention trial. Clin Chem Lab Med 2007;45(12):1582-5.
Stabler SP. Clinical practice. Vitamin B12 deficiency. New Engl J Med. 2013;368(2):149–60.
Tiemeier H, van Tuijl HR, Hofman A, Meijer J, Kilaan AJ, Breteler MM. Vitamin B12, folate, and homocysteine in depression: the Rotterdam study. Arch Gen Psychiatry. 2002; 159:2099-2101
Vargas-Ruiz AG, Hernández-Rivera G, Herrera MF. Prevalence of iron, folate, and vitamin B12 deficiency anemia after laparoscopic Roux-en-Y gastric bypass. Obes Surg. 2008;18(3):288–93.
Walker JG, Batterham PJ, Mackinnon AJ, Jorm AF, Hickie I, Fenech M, Kljakovic M, Crisp D, Christensen H. Oral folic acid and vitamin B-12 supplementation to prevent cognitive decline in community-dwelling older adults with depressive symptoms — the Beyond Ageing Project: a randomized controlled trial. Amer J Clin Nutr. 2012;95(1):194–203.
Wang H, Wahlin Å, Basun H, Fastbom J. Vitamin B 12 and folate in relation to the development of Alzheimer’s disease. Neurology. 2001; 56(9);1188-94.
Werder SF. Cobalamin deficiency, hyperhomocysteinemia, and dementia. Neuropsychiatr Dis Treat. 2010;6:159–95.