Cervical dysplasia and andhuman papilloma virus(HPV)
Nutritional therapeutic management
There are 15 known oncogenic strains of HPV that cause virtually all cases of cervical cancer and cervical dysplasia (Wheeler 2007). Strain 16 and 18 are the high- risk types most commonly detected by cytologic screening. Cervical cancer is the second major cause of cancer deaths among women worldwide, and ranks fourteenth amongst leading causes of cancer in women in the US (Marianne 2010).
Certain cofactors aff ecting the progression of cervical dysplasia to cancer include; long term use of oral contraceptives, multiple sexual partners, poor nutritional status and smoking. All of these factors alter epithelial diff erentiation, cell growth and apoptosis of tumor cells (Gariglio 2009). Addressing the risk factors of cervical cancer broadens the spectrum of treatment options available. This article focuses on various nutrient intervention options, and their safety and efficacy based on human trials as well as biological plausibility.
Nutritional Intervention -when to begin
When a Pap test comes back with minor histologic or cytologic abnormalities, such as atypical squamous cells of undetermined significance (ASCUS), grade 1 cervical intraepithelial neoplasia (CIN1) or low-grade squamous intraepithelial lesion (LSIL), conventional medicine suggests to watch, wait, and repeat the Pap smear. Most of these cytologic changes are associated with HPV infection. It is during this time that nutritional interventions would be appropriate, supporting the immune system to reverse the low-grade cervical cell abnormalities and/or eliminate the associated HPV infection.
Nutritional Medicines
Carotenoids
Carotenoids include beta-carotene, alpha-carotene, cryptoxanthin, gamma-carotene, zeaxanthin, lutein, and lycopene. Studies have shown that beta-carotene deficiency in the cervical cells plays an etiologic role in the development of cervical dysplasia (Palan 1992). In addition, a significant decrease in plasma beta-carotene levels is found in women with either cervical dysplasia or cervical cancer (VanEenwyk 1991).
Carotenoids like lycopene, found in tomatoes, are believed to be more responsible for an improvement in dysplasia than is betacarotene (Palan 1992). A case control trial including 235 women compared healthy controls to women with histopathological diagnosis of cervical intraepithelial neoplasia (CIN) or cervical cancer (Palan 2006). Cases were demonstrated to possess significantly lower plasma levels of lycopene, retinol, cantaxanthin, α-tocopherol and γ-tocopherol. These antioxidants have been shown to protect DNA from oxidative damage and obviate genotypic mutations linked to cancer (Davidson 1992, Witz 1991). Lycopene acts as a quencher of singlet oxygen (Di Mascio 1989).
Results of a Japanese group study on HPV (Nagata 1999) show that the highest tertile of serum lycopene was correlated with decreased risk of cervical dysplasia after observation of blood samples and cervical cells from 156 women. Women with higher plasma cis-lycopene levels were found to have 56% reduction in HPV persistence when compared to women with low levels.
Indole-3-Carbinol (I3C) and 3-3’Diindolylmethane (DIM)
Glucosinolates are compounds that are present in all members of the cruciferous vegetable family, including cabbage, broccoli, brussels sprouts, cauliflower, and kale. They are hydrolyzed by the plant enzyme myrosinase to yield isothiocyanates, which then break down to the metabolites indole-3-carbinol (I3C) and sulphoraphane (Higdon 2007). Research indicates that I3C has the potential to prevent and may treat a number of common cancers, particularly those that are estrogen related (Aubron 2003). Most animal and human studies using I3C to treat cancer show a chemoprotective effect. In a double-blind, placebo-controlled study, 30 patients with biopsy-confirmed CIN II-III were randomized to receive placebo or 200 or 400 mg oral I3C daily for 12 weeks. Four of eight patients in the 200 mg/day group and four of nine in the 400 mg/day group had complete regression of CIN while none in placebo group experienced regression (Bell 2000).
The results of I3C on cervical dysplasia are promising, however safety data from animal models demonstrate that I3C can both inhibit and promote carcinogenesis depending on the species, carcinogen, target organ, and exposure (Reed 2006). Several animal studies have shown a tumor-promoting effect of I3C in the liver, thyroid and endometrium (Kim 1997, Stoner 2002). Additionally, undesirable side effects of I3C include dizziness, unsteady gait and symptoms of nervous system toxicity at only two to three times the normal dose (Rosen 1998).
DIM supplementation, a dimer of I3C, is considered a promising alternative to I3C for its chemoprotective properties and excellent safety profile. However, in 2010, an RCT was conducted on 64 Patients diagnosed with CIN II or CIN III randomized in a 2:1 manner to receive DIM orally at 2mg/kg/day or placebo for 12 weeks. There was no statistically significant difference in any outcome measure between the DIM intervention group and control after six months of regular follow-up (Del Priore 2010).
Dietary intervention with three to five servings of cruciferous vegetables daily is a safe alternative to intervention with I3C. Broccoli sprouts are a rich source of inducers of enzymes that protect against carcinogens, and they have been found to contain 10–100 times more inducer activity than mature cruciferous vegetables (Fahey 1997).
Folic acid (Vitamin B9)
Although studies have revealed folate deficiency as a risk factor for cervical dysplasia, clinical trials with oral folic acid supplements have demonstrated conflicting results. Three hundred and thirty one women with biopsy proven atypia, mild CIN or moderate CIN were randomized to receive either 5 mg of folic acid or placebo orally per day for six months. Colposcopy, Pap smear and serum vitamin levels were monitored every three months. At the end of treatment, there was no significant difference between the treatment group and the control, suggesting that folic acid supplementation does not induce regression of early epithelial cervical abnormalities (Flately 2009). Similar observation was made by Zarcone et al (1996) from a study involving 154 patients with CIN I and CIN II who were randomized to 10 mg of folic acid or placebo for six months orally. After treatment, dysplasia status, biopsy status and prevalence of HPV 16 infection did not differ significantly which suggests that folic acid supplements do not alter the course of established disease.
Hernandez et al (2003) demonstrated that folate from food and supplements have inverse dose-response associations with squamous intraepithelial lesions of the cervix (SIL), in a case control study with 271 controls and 214 women confirmed for high and low grade SIL. Tong et al (2011) found that low serum folate concentration among individuals with methylenetetrahydrofolate reductase variants was coupled with high risk of cervical cancer. It remains unclear whether folic acid is an effective intervention of cervical dysplasia or whether it simply serves as a biomarker of intake of leafy green vegetables.
Vitamin B12
Vitamin B12 studies on HPV persistence and cervical neoplasia have yielded conflicting results. A study comprising 91 low income Hispanic women showed no association between vitamin B12 and risk of HPV persistence (Sedjo 2003). However, lower vitamin B12 levels combined with polymorphisms in the methylenetetrahydrofolate reductase gene were associated with higher risk of cervical cancer (Sedjo 2002). Vitamin B12 is an essential vitamin involved in methylation reactions, fatty acid metabolism, DNA and RNA synthesis. A diet rich in vitamin B12 containing foods or supplemental vitamin B12 may be protective against HPV persistence.
Vitamin C
A randomized study administered 500 mg vitamin C daily (oral) to 141 women confirmed for CIN or squamous atypia (Mackerras 1999). The authors concluded that vitamin C supplements are unlikely to increase the regression or decrease the progression of minor atypia and CIN I. A group of 169 participants with 87 confirmed cervical cancer patients and 82 controls were administered 80 mg and 107 mg of vitamin C respectively. This study demonstrated a ten-fold increase in risk of cervical dysplasia when the intake of vitamin C was 50% less than the recommended daily allowance (Wassertheil-Smoller 1981). A study by Giuliano et al (2003) showed that risk of type-specific persistent HPV infection was lower among women whose intake of vitamin C is higher compared to those in the lowest quartile. Similar results have been reproduced elsewhere (VanEenwyk 1991). Although conflicting reports on vitamin C supplementation exist, it is evident that low vitamin C status is consistently associated with cervical cancer and its precursors.
Vitamin E
Vitamin E exists in eight different forms, four tocopherols and four tocotrienols. with α-tocopherol being the form of vitamin E that is preferentially absorbed and stored in humans. α-tocopherol in a vitamin E rich diet behaves as peroxy radical scavenger with chain breaking properties, inhibiting induced neoplastic transformation of cells (Rigotti 2007). Serum tocopherol levels were found to be low in patients with HPV persistence in a study done with 405 Brazilian women (Siegel 2007).
Prostaglandins are often related to carcinogenic events on account of their ability to suppress the immune system. Vitamin E inhibits prostaglandin action by reducing the adenylate cyclase response to prostaglandins (Stoll 1994). In a study involving American Indian women with biopsy proven CIN I or CIN II/III and same population controls, Yeo et al (2000) reported that low serum α-tocopherol was associated with increased CIN I/III, but the adjusted odds ratio was not significant. Further large cohort studies are needed to assess the role of vitamin E in HPV infection.
Green tea extract (Camelia sinensis)
The FDA approved a topical herbal drug (Polyphenol E) comprised of catechins from green tea leaves to treat genital warts caused by low risk HPV, strains 6 and 11. The efficacy and safety of Polyphenon E was confirmed by a randomized trial on 397 adults with HPV genital warts. Subjects who applied the treatment three times a day had complete clearance of warts in 16 weeks (Stockfleth 2008).
Ahn et al (2003) reviewed the clinical efficacy of green tea extracts in the form of ointment or capsules in treating patients with HPV infected cervical lesions. A cohort of 51 patients with cervical lesions was divided into 4 groups and 39 patients were untreated controls. A 69% response was observed for treatment with green tea extract compared to a 10% response in untreated controls, suggesting that green tea extract can serve as a potential therapy for patients with HPV associated cervical lesions.
Curcuma longa
Curcumin, a yellow pigment from rhizomes of turmeric has been observed to have anticancer properties. Maher et al (2011) analyzed the effects of curcumin on HPV pathways involved in the development of cervical cancer. Curcumin was found to inhibit the transcription of HPV 16, restore the expression of tumor suppressor protein P53, and suppress the growth of cervical cancer cells.
A study by Cheng et al (2001) demonstrated that curcumin is not toxic to humans at doses up to 8000 mg/day when administered orally for three months. This study also showed that curcumin led to histologic improvement in patients with CIN and other premalignant lesions, suggesting a biologic eff ect of curcumin in the chemoprevention of cervical cancer (Maher 2011).
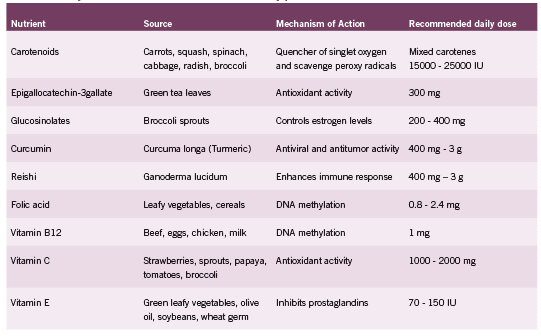
Ganoderma Lucidum
Ganoderma lucidum, known by its common name Reishi mushroom, is traditionally used in Chinese medicine for infl ammation and immunity. Preclinical studies by Gao et al (2003) suggested that the Ganoderma lucidum polysaccharides (GLPS) are responsible for the immune-stimulating eff ects of the herb. ey investigated the eff ects of GLPS on the immune function of 34 advanced-stage cancer patients. ese patients were treated with 1800 mg, three times/day orally for 12 weeks. irty patients after 12 weeks of treatment were assessed for immune function and found to have increased plasma concentrations of IL-2, IL-6 and Interferon gamma and decreased IL-1 and Tumor necrosis factor (TNF) concentrations. e study also found increased NK cell activity after 12 weeks of treatment, indicating that Ganoderma lucidum polysaccharides enhanced the immune response of patients with advanced cancer.
Trametes Versicolor (Previously known as Coriolus versicolor)
Trametes is a mushroom commonly used in Asia for boosting the immune system. Most of the research on this mushroom has focused on its immune-enhancing properties in cancer patients undergoing chemotherapy. Recently, it has been studied for its immunomodulating eff ects on HPV. A study by J. Silva Couto (2006) examined women with CIN I associated with HPV. Half of the women were given 3g/day of Coriolus for a year and the other half received no supplementation. e study found that Coriolus versicolor supplementation over a period of one year substantially increased regression of dysplasia (regression rate 72% vs 47.5%) and induced clearance of the high-risk subtypes of the HPV virus (regression rate 90% vs 8.5%).
Conclusion
Nutritional therapeutic interventions can restore balance to the immune system, tune up the body’s defense against infection and correct nutrient defi ciencies. Nutrient supplementation is an alternative approach to the conventional “watch and wait” approach in response to cervical dysplasia and HPV infection. Supplementation is most eff ective in people with low baseline status of nutritional adequacy. Evidence from human clinical trials suggests that achieving nutrient adequacy exerts a protective eff ect against persistent HPV infection and that dietary and nutritional interventions may prevent the development of cervical dysplasia, or reverse existing histopathological abnormality.
References
Ahn WS, Yoo J, Huh SW, Kim CK, Lee JM, Namkoong SE, Bae SM, Lee IP. Protective effects of green tea extracts (polyphenon E and EGCG) on human cervical lesions. Eur J Cancer Prev. 2003 Oct;12(5):383-90.
Auborn KJ, Fan S, Rosen EM, Goodwin L, Chandraskaren A, Williams DE, Chen D, Carter TH. Indole-3-carbinol is a negative regulator of estrogen. J Nutr. 2003 Jul;133(7 Suppl):2470S-2475S.
Bell MC, Crowley-Nowick P, Bradlow HL, Sepkovic DW, Schmidt-Grimminger D, Howell P, Mayeaux EJ, Tucker A, Turbat-Herrera EA, Mathis JM. Placebocontrolled trial of indole-3-carbinol in the treatment of CIN. Gynecol Oncol. 2000 Aug;78(2):123-9.
Cheng AL, Hsu CH, Lin JK, Hsu MM, Ho YF, Shen TS, Ko JY, Lin JT, Lin BR, Ming- Shiang W, Yu HS, Jee SH, Chen GS, Chen TM, Chen CA, Lai MK, Pu YS, Pan MH, Wang YJ, Tsai CC, Hsieh CY. Phase I clinical trial of curcumin, a chemopreventive agent, in patients with high-risk or pre-malignant lesions. Anticancer Res. 2001 Jul- Aug;21(4B):2895-900.
Couto JS. Evaluation of Coriolus versicolor supplementation in LSIL HPV patients. Townsend Letter: The Examiner of Alternative Medicine. Nov issue 2006.
Davidson SE, West CM, Hunter RD. Lack of association between in vitro clonogenic growth of human cervical carcinoma and tumour stage, differentiation, patient age, host cell infiltration or patient survival. Int J Cancer. 1992 Jan 2;50(1):10-4.
Del Priore G, Gudipudi DK, Montemarano N, Restivo AM, Malanowska-Stega J, Arslan AA. Oral diindolylmethane (DIM): pilot evaluation of a nonsurgical treatment for cervical dysplasia. Gynecol Oncol. 2010 Mar;116(3):464-7.
Di Mascio P, Kaiser S, Sies H. Lycopene as the most efficient biological carotenoid singlet oxygen quencher. Arch Biochem Biophys. 1989 Nov 1;274(2):532-8.
Fahey JW, Zhang Y, and Talalay P. Broccoli sprouts: An exceptionally rich source of inducers of enzymes that protect against chemical carcinogens. Proc Natl Acad Sci USA. 1997 Sept; 94(19): 10367–10372.
Flatley JE, McNeir K, Balasubramani L, Tidy J, Stuart EL, Young TA, Powers HJ. Folate status and aberrant DNA methylation are associated with HPV infection and cervical pathogenesis. Cancer Epidemiol Biomarkers Prev. 2009 Oct;18(10):2782-9.
Gao Y, Zhou S, Jiang W, Huang M, Dai X. Effects of ganopoly (a Ganoderma lucidum polysaccharide extract) on the immune functions in advanced-stage cancer patients. Immunol Invest. 2003 Aug;32(3):201-15.
Gariglio P, Gutierrez J, Cortes E, Vazquez J. The role of retinoid deficiency and estrogens as cofactors in cervical cancer. Arch Med Res. 2009 Aug;40(6):449-65.
Hernandez BY, McDuffie K, Wilkens LR, Kamemoto L, Goodman MT. Diet and premalignant lesions of the cervix: evidence of a protective role for folate, riboflavin, thiamin, and vitamin B12. Cancer Causes Control. 2003 Nov;14(9):859-70.
Higdon JV, Delage B, Williams DE, Dashwood RH. Cruciferous vegetables and human cancer risk: epidemiologic evidence and mechanistic basis. Pharmacol Res. 2007 Mar;55(3):224-36.
Kim DJ. Enhancement by indole-3-carbinol of liver and thyroid gland neoplastic development in a rat medium-term multiorgan carcinogenesis model. Carcinogenesis. 1997. 18 (2): 377-381.
Mackerras D, Irwig L, Simpson JM, Weisberg E, Cardona M, Webster F, Walton L, Ghersi D. Randomized double-blind trial of beta-carotene and vitamin C in women with minor cervical abnormalities. Br J Cancer. 1999 Mar;79(9-10):1448-53.
Maher DM, Bell MC, O’Donnell EA, Gupta BK, Jaggi M, Chauhan SC. Curcumin suppresses human papillomavirus oncoproteins, restores p53, Rb, and PTPN13 proteins and inhibits benzo[a]pyrene-induced upregulation of HPV E7. Mol Carcinog. 2011 Jan;50(1):47-57.
Marianne M. Management of cervical dysplasia and human papillomavirus. Townsend Letter, April issue. 2010.
Nagata C, Shimizu H, Yoshikawa H, Noda K, Nozawa S, Yajima A, Sekiya S, Sugimori H, Hirai Y, Kanazawa K, Sugase M, Kawana T. Serum carotenoids and vitamins and risk of cervical dysplasia from a case-control study in Japan. Br J Cancer. 1999 Dec;81(7):1234-7.
Palan PR, Mikhail MS, Basu J, Romney SL. Beta-carotene levels in exfoliated cervicovaginal epithelial cells in cervical intraepithelial neoplasia and cervical cancer. Am J Obstet Gynecol. 1992 Dec;167(6):1899-903.
Palan PR, Mikhail MS, Goldberg GL, Basu J, Runowicz CD, Romney SL. Plasma levels of beta-carotene, lycopene, canthaxanthin, retinol, and alpha- and tautocopherol in cervical intraepithelial neoplasia and cancer. Clin Cancer Res. 1996 Jan;2(1):181-5.
Reed GA, Arneson DW, Putnam WC, Smith HJ, Gray JC, Sullivan DK, Mayo MS, Crowell JA, Hurwitz A. Single-dose and multiple-dose administration of indole- 3-carbinol to women: pharmacokinetics based on 3,3’-diindolylmethane. Cancer Epidemiol Biomarkers Prev. 2006 Dec;15(12):2477-81.
Rigotti A. Absorption, transport, and tissue delivery of vitamin E. Mol Aspects Med. 2007 Oct-Dec;28(5-6):423-36.
Rosen CA, Woodson GE, Thompson JW, Hengesteg AP, Bradlow HL. Preliminary results of the use of indole-3-carbinol for recurrent respiratory papillomatosis. Otolaryngol Head Neck Surg. 1998 Jun;118(6):810-5.
Sedjo RL, Fowler BM, Schneider A, Henning SM, Hatch K, Giuliano AR. Folate, vitamin B12, and homocysteine status. findings of no relation between human papillomavirus persistence and cervical dysplasia. Nutrition. 2003 Jun;19(6):497-502.
Sedjo RL, Inserra P, Abrahamsen M, Harris RB, Roe DJ, Baldwin S, Giuliano AR. Human papillomavirus persistence and nutrients involved in the methylation pathway among a cohort of young women. Cancer Epidemiol Biomarkers Prev. 2002 Apr;11(4):353-9.
Siegel EM, Craft NE, Duarte-Franco E, Villa LL, Franco EL, Giuliano AR. Associations between serum carotenoids and tocopherols and type-specific HPV persistence: the Ludwig-McGill cohort study. Int J Cancer. 2007 Feb 1;120(3):672-80.
Stoll KE, Ottino P, Duncan JR. Interrelationship of ascorbate, arachidonic acid and prostaglandin E2 in B16 melanoma cells. Prostaglandins Leukot Essent Fatty Acids. 1994 Mar;50(3):123-31.
Stockfleth E, Beti H, Orasan R, Grigorian F, Mescheder A, Tawfik H, Thielert C. Topical Polyphenon E in the treatment of external genital and perianal warts: a randomized controlled trial. Br J Dermatol. 2008 Jun;158(6):1329-38.
Stoner G, Casto B, Ralston S, Roebuck B, Pereira C, Bailey G. Development of a multi-organ rat model for evaluating chemopreventive agents: efficacy of indole-3- carbinol. Carcinogenesis. 2002 Feb;23(2):265-72.
Tong SY, Lee JM, Song ES, Lee KB, Kim MK, Yun YM, Lee JK, Son SK, Lee JP, Kim JH, Hur SY, Kwon YI. The effects of polymorphisms in methylenetetrahydrofolate reductase (MTHFR), methionine synthase (MTR), and methionine synthase reductase (MTRR) on the risk of cervical intraepithelial neoplasia and cervical cancer in Korean women. Cancer Causes Control. 2010 Jan;21(1):23-30.
VanEenwyk J, Davis FG, Bowen PE. Dietary and serum carotenoids and cervical intraepithelial neoplasia. Int J Cancer. 1991 Apr 22;48(1):34-8.
Wassertheil-Smoller S, Romney SL, Wylie-Rosett J, Slagle S, Miller G, Lucido D, Duttagupta C, Palan PR. Dietary vitamin C and uterine cervical dysplasia. Am J Epidemiol. 1981 Nov;114(5):714-24.
Wheeler C. Advances in primary and secondary interventions for cervical cancer: prophylactic human papillomavirus vaccines and testing. Nat Clin Pract Oncol. 2007 Apr: 4(4):224-235.
Witz G. Active oxygen species as factors in multistage carcinogenesis. Proc Soc Exp Biol Med. 1991 Nov;198(2):675-82.
Yeo AS, Schiff MA, Montoya G, Masuk M, van Asselt-King L, Becker TM. Serum micronutrients and cervical dysplasia in Southwestern American Indian women. Nutr Cancer. 2000;38(2):141-50.
Zarcone R, Bellini P, Carfora E, Vicinanza G, Raucci F. [Folic acid and cervix dysplasia]. Minerva Ginecol. 1996 Oct;48(10):397-400.









