Soy and blood lipids
Historical perspective and future directions
The evolution of soy
Soy has been a staple food in the diets of Asian populations for many centuries. In the latter half of the 20th century, North Americans began consuming soy foods on a larger scale, embracing this high-quality protein source as an alternative to animal products high in saturated fats (Messina 2010).
Soy continued to grow in popularity through the 1980’s and 1990’s as evidence of its health benefits began to mount. Research on soy’s active constituents continues to the present day.
A 1995 meta-analysis of the impact of soy foods on cholesterol levels seemed certain to cement soy’s place in a health-promoting diet. This synthesis of published trials reported that consuming an average of 47 grams of soy protein per day could reduce total cholesterol (TC) by 0.60mmol/L (9.3%), low-density lipoprotein (LDL) by 0.56mmol/L (12.9%) and triglycerides (TG) by 0.15mmol/L (10.5%) in hypercholesteremic individuals. At this dose, a non-significant increase in high-density lipoprotein (HDL) of 0.03mmol/L (2.4%) was also observed (Anderson 1995).
FDA and AHA endorsements of soy protein In 1999, the US Food and Drug Administration (FDA) added its voice to the growing acclaim for this humble legume. Soy protein was approved for a health claim to reduce the risk of cardiovascular disease at a daily dose of >25g (Food and Drug Administration 1999). The American Heart Association (AHA) soon followed suit, encouraging the use of soy protein in cholesterol-lowering diets (Erdman 2000), and suggesting that a decrease of 4-8% in LDL levels could be expected with a daily dose of 25-50g. Populationbased studies also indicated a role for soy in the management of lipid levels (Ho 2000).
A period of intense scrutiny has followed in the decade since the FDA approval of the health claim for soy. Subsequent reviews have produced inconsistent results a far smaller magnitude of benefit than that reported in Anderson’s meta-analysis (Weggemans 2003, Zhan 2005). Given this incongruence, the AHA re-evaluated its position on the matter tempering its endorsement of soy, and calling its benefits “minimal at best” in a later statement (Sacks 2006).
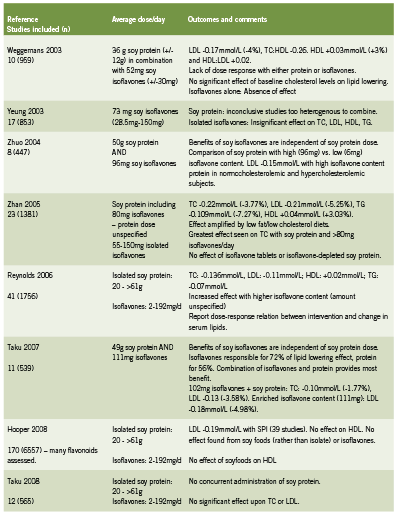
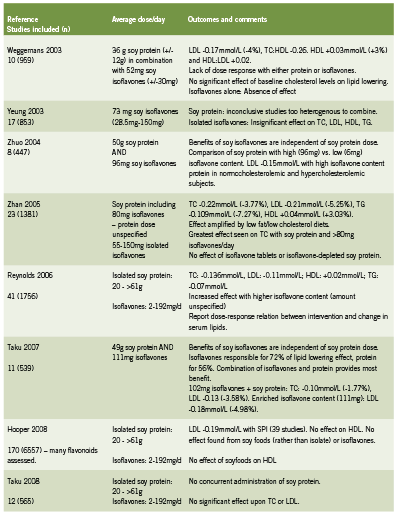
An appraisal of meta-analyses published after 1995 reveals that while the benefit of soy consumption may not be as dramatic as originally reported, some positive effect on blood lipids can still be expected from this intervention (Table 1).
Amplification of past results
Although these studies suggest a trend towards improved lipid profiles, the findings are inconsistent. Some studies show benefit for all parameters (Reynolds 2006, Weggemans 2003, Zhan 2005) while others demonstrate no significant effects (Yeung 2003, Taku 2008). Still others indicate a positive response in some measures, namely LDL and TC (Hooper 2008, Taku 2007, Zhuo 2004). None of the studies were able to replicate the results reported by the original meta-analysis (Anderson 1995).
A survey of the disparities between studies of the past and present reveals some important confounding factors. These issues may be responsible for both an amplification of earlier results, and for a comparative reduction in effect of later research. They include:
• Control diets: Treatment diets in some earlier studies were hypocaloric in comparison to controls, resulting in weight loss (Sacks 2006). Others were not matched to controls in terms of dietary fat, fibre and cholesterol content (Weggemans 2003). Recent studies equalize treatment and control diets more carefully (Taku 2008, Zhuo 2004). As weight loss (Dutheil 2010), fibre (Bruckert 2011) and decreased cholesterol intake (Stalenhoef 1997) may independently improve lipid levels, the benefits of soy may have been overestimated as a result of additive effects from these other variables in the treatment diet.
• Participants: Study subjects in early studies were primarily men and pre-menopausal women (Dewell 2006), while more recent studies have included many more post-menopausal women (Zhan 2005, Zhuo 2004). Recent RCTs have failed to show benefit in post-menopausal women (Beavers 2010, Campbell 2010). Reported associations between menopausal status and lipid levels suggest that hormonal factors contribute to dyslipidemia in post-menopausal women (Agrinier 2009). Hormonallyinfluenced dyslipidemia could theoretically be resistant to soy treatment, possibly contributing to the more modest results of recent studies.
• Baseline lipid measurements: Although the results of the Anderson meta-analysis are widely quoted as they appear above, only participants with moderate hypercholesterolemia (6.70 to 8.61 mmol/L) at baseline experienced this degree of change (Anderson 1995). Recent meta-analyses have confirmed this association between baseline cholesterol levels and the magnitude of effect (Reynolds 2006, Zhan 2005), although others have found no such relationship (Weggemans 2003, Zhuo 2004). The impressive results from the Anderson study continue to be quoted with no mention of baseline cholesterol status (Campbell 2010, Thorp 2008), resulting in an inaccurate description of effect.
Divergent conclusions from current soy trials (Borodin 2009, Shidfar 2009; Beavers 2010) suggest that other confounding factors have yet to be identified. Variations in soy isoflavone content, equol producer status and manufacturing standards may be partly responsible for these contraditory results.
Soy protein and soy isoflavones
Public statements by both the FDA (1999) and the AHA (Erdman 2000) indicate that soy protein is the agent responsible for lipidlowering, rather than any of the plant’s native isoflavones, which include genistein and daidzein. Studies have tended to show that isoflavones given in isolation have little impact on lipid fractions (Hooper 2008, Taku 2008, Weggemans 2003, Yeung 2003). While this may be true, a case can be made for a synergistic effect between soy protein and soy isoflavones.
The four meta-analyses presented in Table 1 that examined soy isoflavones given in combination with soy protein found benefit from these interventions (Reynolds 2006, Taku 2007, Zhan 2005, Zhuo 2004). Each team further concluded that lipid-lowering is enhanced when doses of isoflavones are highest, although no consistent minimum intake was established.
A hypolipidemic effect has yet to be attributed to any one isoflavone. Older studies on soy provide limited information about specific isoflavone content (Weggemans 2003), creating an opportunity for future research.
Equol producer/non-producer status
Should isoflavones prove to play a role in lipid metabolism in the presence of soy protein, the question of equol status must be addressed. Equol is the active metabolite of daidzein, and can be produced by approximately 30% of the adult population in Western countries (Setchell 2010).
In studies of isoflavones for the management of menopausal symptoms, equol producers tend to show greater response to the intervention (Jou 2008). The same may be true of isoflavones and lipid levels (Cassidy 2006, Taku 2007, Weggemans 2003, Zhuo 2004), although isolated RCTs have yet to demonstrate increased effect in equol producers (Thorp 2008).
Manufacturing concerns
Future studies may conclude that a soy-based storage protein, 7S globulin, is responsible for the hypocholesteremic effect of soy. 7S globulin has been shown to upregulate LDL uptake and degradation in vitro (Lovati 2000).
In comparisons of high- and low-isoflavone soy proteins, ethanol is used to remove isoflavones from soy product (Zhuo 2004). Studies of ethanol-processed soy reveal a marked reduction of 7S globulin and other molecules (Gianazza 2003), which could explain the decreased effect of isoflavone-poor soy protein on blood lipids (Zhan 2005).
Denaturing soy protein through ethanol or heat exposure may even have deleterious effects, as evidenced by a recent study using ultra-heat-treated (UHT) soymilk and control preparations (Hoie 2006). After 4 weeks of supplementation, LDL levels in all subjects increased by an astounding 17-19%.
Dramatically different results were reported when the same investigators evaluated a nondenatured soy protein supplement (Hoie 2007). At the conclusion of the 8-week study, the treatment group experience a decrease in LDL levels of 12.0% (p=0.002), suggesting that manufacturing methods can significantly alter the effect of soy interventions.
Future directions
As our understanding of the mechanisms of soy metabolism evolves, so does our ability to use this intervention in a clinically relevant manner. At present, the evidence supports combining isoflavone-rich, soy protein with other dietary agents such as plant sterols, viscous fibre and nuts to achieve a lipid-lowering effect (Jenkins 2010).
Recent studies suggest reductions in LDL levels of approximately 3-5% may be expected from nondenatured soy protein in doses ranging from 20-60g per day. Studies suggest that an isoflavone content of at least 80mg is associated with benefit (Zhan 2005). Additional reductions of up to 6% may occur if soy protein displaces animal protein in the diet (Jenkins 2010). An increase in HDL of 3% and a decrease in TC of 2-4% may also be associated with soy consumption (Reynolds 2006, Taku 2007, Weggemans 2003, Zhan 2005).
Many clinically important questions remain regarding the role of soy in the management of cardiovascular disease. Is equol producer status a determinant of effect? Can soy use impact the incidence of cardiovascular accidents or coronary heart disease? Can specific populations including post-menopausal women and individuals with Type 2 diabetes benefit from this intervention? These queries represent essential areas for future research.
References:
Agrinier N, Cournot M, Ferrières J. [Dyslipidemia in women after 50: age, menopause or both?]. Ann Cardiol Angeiol (Paris). 2009 Jun;58(3):159-64. Epub 2008 Oct 14. [Article in French] (abstract only)
Anderson JW, Johnstone BM, Cook-Newell ME. Meta-analysis of the effects of soy protein intake on serum lipids. N Engl J Med. 1995 Aug 3;333(5):276-82.
Beavers KM, Serra MC, Beavers DP, Hudson GM, Willoughby DS. The lipid-lowering effects of 4 weeks of daily soymilk or dairy milk ingestion in a postmenopausal female population. J Med Food. 2010 Jun;13(3):650-6.
Borodin EA, Menshikova IG, Dorovskikh VA, Feoktistova NA, Shtarberg MA, Yamamoto T, Takamatsu K, Mori H, Yamamoto S. Effects of two-month consumption of 30 g a day of soy protein isolate or skimmed curd protein on blood lipid concentration in Russian adults with hyperlipidemia. J Nutr Sci Vitaminol (Tokyo). 2009 Dec;55(6):492-7.
Bruckert E, Rosenbaum D. Lowering LDL-cholesterol through diet: potential role in the statin era. Curr Opin Lipidol. 2011 Feb;22(1):43-8.
Campbell SC, Khalil DA, Payton ME, Arjmandi BH. One-year soy protein supplementation does not improve lipid profile in postmenopausal women. Menopause. 2010 May-Jun;17(3):587- 93.
Cassidy A, Brown JE, Hawdon A, Faughnan MS, King LJ, Millward J, Zimmer-Nechemias L, Wolfe B, Setchell KD. Factors affecting the bioavailability of soy isoflavones in humans after ingestion of physiologically relevant levels from different soy foods. J Nutr. 2006 Jan;136(1):45- 51.
Dewell A, Hollenbeck PL, Hollenbeck CB. Clinical review: a critical evaluation of the role of soy protein and isoflavone supplementation in the control of plasma cholesterol concentrations. J Clin Endocrinol Metab. 2006 Mar;91(3):772-80.
Dutheil F, Lesourd B, Courteix D, Chapier R, Dore E, Lac G. Blood lipids and adipokines concentrations during a 6 months nutritional and physical activity intervention for metabolic syndrome treatment. Lipids Health Dis. 2010 Dec 31;9(1):148.
Erdman JW Jr. AHA Science Advisory: Soy protein and cardiovascular disease: A statement for healthcare professionals from the Nutrition Committee of the AHA. Circulation. 2000 Nov 14;102(20):2555-9.
Food and Drug Administration. Food labelling: health claims; soy protein and coronary heart disease. Fed Regist. 1999; 64:577000-33.
Gianazza E, Eberini I, Arnoldi A, Wait R, Sirtori CR. A proteomic investigation of isolated soy proteins with variable effects in experimental and clinical studies. J Nutr. 2003 Jan;133(1):9-14.
Ho SC, Woo JL, Leung SS, Sham AL, Lam TH, Janus ED. Intake of soy products is associated with better plasma lipid profiles in the Hong Kong Chinese population. J Nutr. 2000 Oct;130(10):2590-3.
Hoie LH, Guldstrand M, Sjoholm A, Graubaum HJ, Gruenwald J, Zunft HJ, Lueder W. Cholesterol-lowering effects of a new isolated soy protein with high levels of nondenaturated protein in hypercholesterolemic patients. Adv Ther. 2007 Mar-Apr;24(2):439-47.
Hoie LH, Sjoholm A, Guldstrand M, Zunft HJ, Lueder W, Graubaum HJ, Gruenwald J. Ultra heat treatment destroys cholesterol-lowering effect of soy protein. Int J Food Sci Nutr. 2006 Nov-Dec;57(7-8):512-9.
Hooper L, Kroon PA, Rimm EB, Cohn JS, Harvey I, Le Cornu KA, Ryder JJ, Hall WL, Cassidy A. Flavonoids, flavonoid-rich foods, and cardiovascular risk: a meta-analysis of randomized controlled trials. Am J Clin Nutr. 2008 Jul;88(1):38-50.
Jenkins DJ, Mirrahimi A, Srichaikul K, Berryman CE, Wang L, Carleton A, Abdulnour S, Sievenpiper JL, Kendall CW, Kris-Etherton PM. Soy protein reduces serum cholesterol by both intrinsic and food displacement mechanisms. J Nutr. 2010 Dec;140(12):2302S-2311S.
Jou HJ, Wu SC, Chang FW, Ling PY, Chu KS, Wu WH. Effect of intestinal production of equol on menopausal symptoms in women treated with soy isoflavones. Int J Gynaecol Obstet. 2008 Jul;102(1):44-9.
Lovati MR, Manzoni C, Gianazza E, Arnoldi A, Kurowska E, Carroll KK, Sirtori CR. Soy protein peptides regulate cholesterol homeostasis in Hep G2 cells. J Nutr. 2000 Oct;130(10):2543-9.
Messina M. A brief historical overview of the past two decades of soy and isoflavone research. J Nutr. 2010 Jul;140(7):1350S-4S.
Reynolds K, Chin A, Lees KA, Nguyen A, Bujnowski D, He J. A meta-analysis of the effect of soy protein supplementation on serum lipids. Am J Cardiol. 2006 Sep 1;98(5):633-40.
Sacks FM, Lichtenstein A, Van Horn L, Harris W, Kris-Etherton P, Winston M; American Heart Association Nutrition Committee. Soy protein, isoflavones, and cardiovascular health: an American Heart Association Science Advisory for professionals from the Nutrition Committee. Circulation. 2006 Feb 21;113(7):1034-44.
Setchell KD, Clerici C. Equol: history, chemistry, and formation. J Nutr. 2010 Jul;140(7):1355S-62S. Epub 2010 Jun 2.
Shidfar F, Ehramphosh E, Heydari I, Haghighi L, Hosseini S, Shidfar S. Effects of soy bean on serum paraoxonase 1 activity and lipoproteins in hyperlipidemic postmenopausal women. Int J Food Sci Nutr. 2009 May;60(3):195-205.
Stalenhoef AF. [Cholesterol reducing food certainly is useful]. Ned Tijdschr Geneeskd. 1997 Dec 27;141(52):2543-5.(abstract)
Taku K, Umegaki K, Ishimi Y, Watanabe S. Effects of extracted soy isoflavones alone on blood total and LDL cholesterol: Meta-analysis of randomized controlled trials. Ther Clin Risk Manag. 2008 Oct;4(5):1097-103.
Taku K, Umegaki K, Sato Y, Taki Y, Endoh K, Watanabe S. Soy isoflavones lower serum total and LDL cholesterol in humans: a meta-analysis of 11 randomized controlled trials. Am J Clin Nutr. 2007 Apr;85(4):1148-56.
Thorp AA, Howe PR, Mori TA, Coates AM, Buckley JD, Hodgson J, Mansour J, Meyer BJ. Soy food consumption does not lower LDL cholesterol in either equol or nonequol producers. Am J Clin Nutr. 2008 Aug;88(2):298-304.
Weggemans RM, Trautwein EA. Relation between soy-associated isoflavones and LDL and HDL cholesterol concentrations in humans: a meta-analysis. Eur J Clin Nutr. 2003 Aug;57(8):940-6.
Yeung J, Yu TF. Effects of isoflavones (soy phyto-estrogens) on serum lipids: a meta-analysis of randomized controlled trials. Nutr J. 2003 Nov 19;2:15.
Zhan S, Ho SC. Meta-analysis of the effects of soy protein containing isoflavones on the lipid profile. Am J Clin Nutr. 2005 Feb;81(2):397-408.
Zhuo XG, Melby MK, Watanabe S. Soy isoflavone intake lowers serum LDL cholesterol: a meta-analysis of 8 randomized controlled trials in humans. J Nutr. 2004 Sep;134(9):2395-400.