FODMAP diet
Implications in irritable bowel syndrone B
Abstract
Most patients with IBS link their symptoms to food consumption. However, the current dietary recommendations for the management of IBS are inconsistent. FODMAPs, a group of short-chain carbohydrates have been identified as aggravating factors in patients with IBS. The constituents under the FODMAP umbrella are discussed. Research exploring the benefit of implementing a low FODMAP diet in patients with IBS is outlined. Recommending a reduction or an elimination of these specific carbohydrates in the diet may provide relief to those suffering with IBS.
Introduction Irritable bowel syndrome (IBS) is a common disease encountered worldwide (Morcos 2009), with a prevalence in Europe and North America between 10-15% (Hungin 2003, Quigley 2009). Typically characterized by either Rome or Manning criteria, irritable bowel syndrome is a chronic, recurring gastrointestinal problem, characterised by abdominal pain, bloating, and changes in bowel habit. Diagnosis is made by exclusion of other causes of organic bowel disease. IBS has a female predominance, often aggregating in families (Spiller 2007), with genetic studies show a connection (Hotoleanu 2008, Saito 2005).
IBS is not associated with an increase in the development of any serious diseases, however patients with IBS suffer from a reduced quality of life, both physically and mentally (Li 2003). Kennedy and Jones (2000) showed that patients with IBS are more likely to undergo surgical operations, including hysterectomy (Kennedy 2000) and cholecystectomy (Kennedy 2000). The financial burden of IBS can be quite significant due to increased medical office visits, diagnostic testing, pharmacotherapy, and emergency room visits (Martin 2001).
Many factors have been hypothesized as playing a role in the pathogenesis of IBS, including, but not limited to; gutbrain axis dysfunction (Bonaz 2009), impaired gut barrier, altered microflora, and low grade immune activation (Cremon 2009). Food intolerances are well known to play a role in the development of IBS symptoms, with patients indentifying a number of different categories of foods like those rich in carbohydrates, as well as fatty foods (Bohn 2013), coffee, alcohol, spicy food (Simren 2001), dairy (Vernia 2004), and gluten (Vazquez-Roque 2013), as common culprits. Between half and two thirds of patients with IBS associate symptoms with eating a meal (Ragnarsson 1998), with gas and abdominal pain as the most frequently reported symptoms (Simren 2001). Implementing elimination diets can be useful, but often patients don’t achieve a significant reduction in symptoms, or during the re-introduction or challenge phase, end up confused with some food reactions, due to the complex mixtures of foods, and timing (Barrett 2012).
Since IBS is so widespread, with multi-factorial causes, and varying consequences, much interest has been paid to finding ways to reduce symptoms and improve the quality of life in sufferers. Despite the lack of conclusive findings of a link between food and IBS, encouraging evidence has prompted further study of dietary modifications.
FODMAP concept and constituents
FODMAP is a relatively new concept, with the phrase being coined by a group of Australian researchers who studied the effects of a seemingly unrelated group of carbohydrates on symptoms of IBS (Gibson 2005, Shepherd 2006). FODMAP stands for fermentable oligosacchardies, disaccharides, monosaccharies, and polyols. The included short chain carbohydrates are fructose, lactose, fructo- and galactooligosaccharides (fructans, and galactans), and polyols (such as sorbitol). The acronym includes short-chain carbohydrates that are poorly absorbed and rapidly fermented, as this is the mechanism by which these carbohydrates induce symptoms. FODMAPs have also been found to be osmotically active (Barrett 2010).
The idea that fructose aggravates digestive system function is not new. Fructose is found in the diet as a free monosaccharide, hexose, as a constituent of the disaccharide sucrose, or in a polymerized form (fructan) (Gibson 2007). A study conducted in 1978 showed that fructose ingestion aggravated abdominal symptoms, and complete elimination of fructose improved symptoms of abdominal pain and colic (Andersson 1978) Absorptive capacity of fructose varies among individuals (Truswell 1988). Free fructose is absorbed by a different transport system than glucose, namely GLUT-5 (Burant 1992), which works more slowly and can be overwhelmed by large amounts of fructose (Truswell 1988). Malabsorption of fructose in healthy individuals, identified by a positive hydrogen breath test, was found in 53% of subjects given a dose of 25 grams, and in 73% of subjects given 50 grams (Beyer 2005). Despite positive breath tests, participants in the study experienced minimal gastrointestinal effects, however, studies have shown that the development of symptoms of fructose malabsorption occur much more readily in patients with IBS, and the use of fructose-free diets have dramatically reduced symptoms (Fernandez- Banares 1993, Goldstein 2000, Symons 1992). In 2008, Shepherd et al conducted a double-blinded, randomized, quadruple arm, placebo-controlled rechallenge trial. They found that symptoms of IBS were not adequately controlled in 70-79% of subjects who received fructose, fructans, or a mixture of the two carbohydrates in the context of diet. Aggravation of symptoms such as abdominal pain, bloating and flatulence occurred as patients were challenged with increasing doses of fructose and/or fructans. When subjects received the placebo, glucose alone, they experienced significantly less severe symptoms, which suggests that dietary restriction of fructose and/or fructans is likely to be responsible for symptomatic improvement.
The question of why a natural sugar found in fruit and other foods has more recently been found to cause digestive system symptoms relates to the increased intake of concentrated fructose. The development of high fructose corn syrup (containing on average 47-65% fructose (Ventura 2011)) and subsequent increase in consumption (Beyer 2005), is hypothesized to be a key factor involved in the increase in fructose malabsorption (Latulippe 2011). The average intake of fructose was thought to be approximately 37 g per day (Park 1993) but was then re-evaluated in 2004 to be 49 g/day (Marriott 2009). This increase in dietary fructose load may more commonly exceed the absorptive capacity of the intestines, exacerbating or unmasking IBS (Shepherd 2006).
Interestingly, fructose absorption is altered depending on glucose presence. As previously mentioned, the absorption mechanism for fructose as a monosaccharide via the GLUT-5 transporter can become saturated. Studies have indicated that when glucose is present, either as free glucose, or when glucose and fructose are combined to form the disaccharide, sucrose, fructose absorptive capacity is increased (Riby 1993) by up-regulation of the GLUT-2 transporter and no malabsorptive state results (Shepherd 2006). This is clinically relevant, as researchers Barrett and Shepherd indicated, because it allows patients to choose foods that are fructose and glucose balanced (e.g. berries and stone fruits) or where glucose is in greater amounts, rather than completely eliminating all fructose containing foods. Another option is to consume glucose with high fructose containing foods, however this could present a problem for blood sugar control.
Fructans are oligosaccharides and polysaccharides of fructose units with a glucose terminal end (Gibson 2007). They are referred to as inulins and fructooligosaccharides (FOS) and are found in foods such as wheat, onions, garlic, artichokes, and chicory. Fructans are completely unabsorbed by upper gastrointestinal tract, and are therefore rapidly fermentable (Rumessen 1998). Fructo-oligosaccharide is a well known prebiotic fibre, that has numerous health benefits, including its ability to increase populations of bacteria in the gut, specifically Bifidobacteria (Gibson 1995). However, research has shown that large amounts (14-20 g) of fructans can aggravate symptoms in people suffering from IBS (Olesen 2000), and can cause digestive upset (especially flatulence) even in healthy individuals (Pedersen 1997, Stone-Dorshow 1987). The average daily intake of fructans via the diet has been calculated to be as much as 10 g/day (van Loo 1995), but with the addition of inulin or FOS to food for its many health benefits, daily intake levels could be greater. Wheat, which accounts for 70% of the daily intake of fructans (Moshfegh 1999), could also be problematic, especially when consumed in large amounts. This may in part explain why gluten elimination has been found to decrease symptoms in individuals who suffer from IBS.
Like fructans, galactans, polymers of galactose, more commonly known as raffinose and styachose, are almost completely unabsorbed in all people, leading to significant fermentation and therefore gas production. Galactans are found in large amounts in legumes, including lentils, chickpeas, kidney beans and have been found to aggravate symptoms of IBS (Chirila 2012), and are therefore included under the FODMAP umbrella.
Lactose is the disaccharide included under the FODMAP umbrella. Lactose absorption depends on the activity of the hydrolase enzyme lactase, which is deficient in 2-100% of people in various populations worldwide (Swagerty 2002). Sixty-eight percent of people with IBS tested positive, via hydrogen breath test, for lactose malabsorption. After adhering to a lactose-free diet, symptoms subsided in nearly half of study participants. Other studies have found similar results (Bohmer 1996), and have suggested that the use of a hydrogen breath test could be used to identify lactose malabsorbers, thus allowing a less strict diet.
Polyols, are sugar alcohols, including; sorbitol, xylitol, mannitol, maltitol, and isomalt, found naturally in some foods and added to many foods as artificial sweeteners. Polyols are incompletely absorbed, and it is well known that sorbitol specifically, has an osmotic laxative effect at high amounts (Hyams 1983). Unlike fructose, polyols do not have an associated active transport system in the small intestine and are probably absorbed by passive diffusion (Gibson 2010). The incomplete absorption of sugar alcohols has been found in healthy controls, at larger doses, indicating a dose response to malabsorption (Corazza 1988). Despite positive hydrogen breath tests, not all malabsorbers displayed symptoms, however, those with IBS experienced significantly more symptoms (Fernandez-Banares 1993, Nelis 1990, Symons 1992)
As evident in the literature, each of the carbohydrate constituents of FODMAPs have been investigated individually. Tests of FODMAPs as a whole have also been conducted, not only by the Australian research group who originally grouped the short-chain carbohydrates together, but increasingly by other researchers worldwide and are showing promising results (Staudacher 2011, Ostgaard 2012, de Roest 2013).
The FODMAP diet in research
Mechanistically the FODMAP diet as a whole has been studied using an ileostomy model, which has been used to study the digestion and absorption of carbohydrates in previous studies (Englyst 1985, Langkilde 1994). Barrett et al (2010) investigated the effect of dietary FODMAPs on the content of water and fermentable substrates of ileal effluent. Individuals with an ileostomy, but no evidence of small intestinal disease, undertook two 4-day dietary periods, comprising diets differing only in FODMAP content. Ileal effluent was collected every two hours on day four of each diet. The FODMAP content of the diet and effluent was measured and patients rated the effluent consistency on a visual analog scale. The effluent of the high FODMAP diet was found to be greater in dry weight and water content. Study participants perceived effluent consistency to be thicker with the low FODMAP diet. The researchers concluded that FODMAPs do increase delivery of water and fermentable substrates to the proximal colon (Barrett 2010). This study was the first mechanism type study that specifically addressed FODMAPs in the diet, as opposed to certain carbohydrates in isolation, confirming that FODMAPs as part of a diet are osmotically active and their poor absorption gives rise to potential fermentation and associated gas production.
It is well known that people suffering from IBS often experience abdominal pain, bloating, and gas due to luminal distension. Ong et al (2010) demonstrated that dietary manipulation of FODMAPs can impact the total amount of gastrointestinal gas production and the spectrum of gas produced (hydrogen vs. methane) in healthy individuals and those with IBS. While an increase in gas was seen even in healthy individuals ingesting a high FODMAP diet, increased gastrointestinal symptoms as well as systemic symptoms, like fatigue, were seen in patients with IBS.
A number of studies have linked the gut microenvironment with the pathophysiology of IBS (Simren 2013). Studies have identified inherent differences in the gut microflora and thus fermentation in IBS patients versus controls (Kassinen 2007, Madden 2002), which could explain the connection with FODMAPs, showing that FODMAPs don’t cause IBS, but could be aggravating symptoms by providing rapidly fermentable substrates to the intestines. Small intestine bacterial overgrowth (SIBO) has been found to be associated with IBS (Sachdeva 2011), and by nature of the FODMAP diet, a reduction in the intake of short-chain carbohydrates, and therefore fermentation, could be useful as dietary treatment.
In a recent study, 90 patients with IBS received dietary advice regarding a low FODMAP diet and completed a hydrogen/methane breath testing for fructose and lactose malabsorption (deRoest 2013). Patients were then asked to complete a questionnaire approximately 15 months later. Results revealed a significant improvement in abdominal pain, bloating, flatulence. The authors concluded that breath testing was a good way to help people understand and adhere to the diet (de Roest 2013). Breath testing has been used and recommended by other researchers as a clinical tool for assessing malabsorption (Barrett 2009, Gibson 2010). Gibson et al (2010) have suggested that breath testing for fructose and lactose malabsorption might be worthwhile because it would allow foods with negative results to be reintroduced back into the diet to a comfortable level, avoiding unnecessary restrictions(Gibson 2010), and providing a source of beneficial prebiotic fibre (Barrett 2012).
Clinical Utility
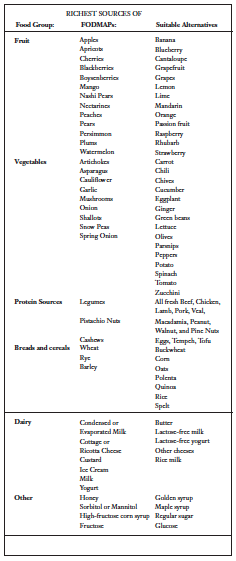
Table 1 (CCS 2012) outlines foods that are high in FODMAPs and suitable alternatives. Since food plays a large role in patient’s perception of symptom induction, many IBS sufferers are potentially already unknowingly avoiding FODMAP foods. The FODMAP diet has been shown to be fairly simple to implement, with limited instruction (Ostgaard 2012). A study by Ostgaard et al (2012) showed that after two hours of dietary guidance by a dietician, patients with IBS avoided all FODMAP‑rich food, consumed more food with probiotic supplements and did not avoid food sources that were crucial to their health. They had improved quality of life and reduced symptoms. Guidance on the management of diet improved their choice of a healthier diet, improved quality of life and reduced IBS symptoms.
Gibson et al (2009) suggest a strict low FODMAP diet for a period of six to eight weeks, followed by a trial of foods to test tolerance, keeping total low FODMAP intake in mind. This would allow patients to occasionally consume foods deemed high FODMAP to a tolerable level, to ensure variety in the diet.
A low FODMAP diet improved symptoms in at least 74% of patients with IBS (Barrett 2012). In the UK, The FODMAP diet was studied in comparison to the UK National Institute for Health and Clinical Excellence (NICE) dietary guidelines for symptom control in patients with IBS. Up to 86% of patients in the FODMAP group experienced overall symptom response, versus 49% in the standard group. Significantly more patients in the low FODMAP group reported improvements in bloating, abdominal pain, and flatulence. This drew the conclusion that a low FODMAP diet is more effective than the standard dietary advice in the UK, for symptom control in IBS (Staudacher 2011). With a continually growing body of evidence, both for the individual constituents of FODMAPs, as well as FODMAPs as a whole, the FODMAP diet seems a reasonable option for dietary management in patients suffering from IBS.
References
Andersson DEH, Nygren A. Four Cases of Long-Standing Diarrhoea and Colic Pains Cured by Fructose-Free diet—A Pathogenetic Discussion. Acta Medica Scandinavica. 1978;203(1- 6):87-92.
Barrett JS. Extending our knowledge of fermentable, short- chain, carbohydrates for managing gastrointestinal symptoms. Nutrition in Clinical Practice. 2013;28(3):300-306.
Barrett JS, Gearry RB, Muir JG, Irving PM, Rose R, Rosella O, Haines ML, Shepherd SJ, Gibson PR. Dietary poorly absorbed, short-chain carbohydrates increase delivery of water and fermentable substrates to the proximal colon. Aliment Pharmacol Ther. 2010 Apr;31(8): 874-882.
Barrett JS, Gibson PR. Fermentable oligosaccharides, disaccharides, monosaccharides and polyols (FODMAPs) and nonallergic food intolerance: FODMAPs or food chemicals? Therap Adv Gastroenterol. 2012 Jul;5(4): 261-268.
Barrett JS, Irving PM, Shepherd SJ, Muir JG, Gibson PR. Comparison of the prevalence of fructose and lactose malabsorption across chronic intestinal disorders. Aliment Pharmacol Ther. 2009 Jul;30(2): 165-174.
Beyer PL, Caviar EM, McCallum RW. Fructose intake at current levels in the United States may cause gastrointestinal distress in normal adults. J Am Diet Assoc. 2005 Oct;105(10): 1559-1566.
Bohmer CJ, Tuynman HA. The clinical relevance of lactose malabsorption in irritable bowel syndrome. Eur J Gastroenterol Hepatol. 1996 Oct;8(10): 1013-1016.
Bohn L, Storsrud S, Tornblom H, Bengtsson U, Simren M. Self-reported food-related gastrointestinal symptoms in IBS are common and associated with more severe symptoms and reduced quality of life. Am J Gastroenterol. 2013 May;108(5): 634-641.
Bonaz B, Sabate JM. Brain-gut axis dysfunction. Gastroenterol Clin Biol. 2009 Feb;33 Suppl 1: S48-58.
Burant CF, Takeda J, Brot-Laroche E, Bell GI, Davidson NO. Fructose transporter in human spermatozoa and small intestine is GLUT5. J Biol Chem. 1992 Jul;267(21): 14523-14526.
CCS, Monash University. The Monash University Low FODMAP Diet. 2012. Melbourne, Australia, Monash University.
Chirila I, Petrariu FD, Ciortescu I, Mihai C, Drug VL. Diet and irritable bowel syndrome. J Gastrointestin Liver Dis. 2012 Dec;21(4): 357-362.
Corazza GR, Strocchi A, Rossi R, Sirola D, Gasbarrini G. Sorbitol malabsorption in normal volunteers and in patients with coeliac disease. Gut. 1988 Jan;29(1): 44-48.
Cremon C, Gargano L, Morselli-Labate AM, Santini D, Cogliandro RF, De Giorgio R, Stanghellini V, Corinaldesi R, Barbara G. Mucosal immune activation in irritable bowel syndrome: gender-dependence and association with digestive symptoms. Am J Gastroenterol. 2009 Feb;104(2): 392-400.
de Roest RH, Dobbs BR, Chapman BA, Batman B, O’Brien LA, Leeper JA, Hebblethwaite CR, Gearry RB. The low FODMAP diet improves gastrointestinal symptoms in patients with irritable bowel syndrome: a prospective study. Int J Clin Pract. 2013 May;epub.
Englyst HN, Cummings JH. Digestion of the polysaccharides of some cereal foods in the human small intestine. The American Journal of Clinical Nutrition. 1985 Nov;42(5): 778-787.
Fernandez-Banares F, Esteve-Pardo M, de Leon R, Humbert P, Cabre E, Llovet JM, Gassull MA. Sugar malabsorption in functional bowel disease: clinical implications. Am J Gastroenterol. 1993 Dec;88(12): 2044-2050.
Gibson GR, Beatty ER, Wang X, Cummings JH. Selective stimulation of bifidobacteria in the human colon by oligofructose and inulin. Gastroenterology. 1995 Apr;108(4): 975-982.
Gibson PR, Newnham E, Barrett JS, Shepherd SJ, Muir JG. Review article: fructose malabsorption and the bigger picture. Aliment Pharmacol Ther. 2007 Feb;25(4): 349-363.
Gibson PR, Shepherd SJ. Personal view: food for thought–western lifestyle and susceptibility to Crohn’s disease. The FODMAP hypothesis. Aliment Pharmacol Ther. 2005 Jun;21(12): 1399- 1409.
Gibson PR, Shepherd SJ. Evidence-based dietary management of functional gastrointestinal symptoms: The FODMAP approach. J Gastroenterol Hepatol. 2010 Feb;25(2): 252-258.
Goldstein R, Braverman D, Stankiewicz H. Carbohydrate malabsorption and the effect of dietary restriction on symptoms of irritable bowel syndrome and functional bowel complaints. Isr Med Assoc J. 2000 Aug;2(8): 583-587.
Hotoleanu C, Popp R, Trifa AP, Nedelcu L, Dumitrascu DL. Genetic determination of irritable bowel syndrome. World J Gastroenterol. 2008 Nov;14(43): 6636-6640.
Hungin AP, Whorwell PJ, Tack J, Mearin F. The prevalence, patterns and impact of irritable bowel syndrome: an international survey of 40,000 subjects. Aliment Pharmacol Ther. 2003 Mar;17(5): 643-650.
Hyams JS. Sorbitol intolerance: an unappreciated cause of functional gastrointestinal complaints. Gastroenterology. 1983 Jan;84(1): 30-33.
Kassinen A, Krogius-Kurikka L, Makivuokko H, Rinttila T, Paulin L, Corander J, Malinen E, Apajalahti J, Palva A. The fecal microbiota of irritable bowel syndrome patients differs significantly from that of healthy subjects. Gastroenterology. 2007 Jul;133(1): 24-33.
Kennedy TM, Jones RH. Epidemiology of cholecystectomy and irritable bowel syndrome in a UK population. Br J Surg. 2000 Dec;87(12): 1658-1663.
Kennedy TM, Jones RH. The epidemiology of hysterectomy and irritable bowel syndrome in a UK population. Int J Clin Pract. 2000 Dec;54(10): 647-650.
Langkilde AM, Andersson H, Schweizer TF, Wursch P. Digestion and absorption of sorbitol, maltitol and isomalt from the small bowel. A study in ileostomy subjects. Eur J Clin Nutr. 1994 Nov;48(11): 768-775.
Latulippe ME, Skoog SM. Fructose malabsorption and intolerance: effects of fructose with and without simultaneous glucose ingestion. Crit Rev Food Sci Nutr. 2011 Aug;51(7): 583- 592.
Li FX, Patten SB, Hilsden RJ, Sutherland LR. Irritable bowel syndrome and health-related quality of life: a population-based study in Calgary, Alberta. Can J Gastroenterol . 2003 Apr;17(4): 259-263.
Madden JA, Hunter JO. A review of the role of the gut microflora in irritable bowel syndrome and the effects of probiotics. Br J Nutr. 2002 Sep;88 Suppl 1:S67-72.
Marriott BP, Cole N, Lee E. National estimates of dietary fructose intake increased from 1977 to 2004 in the United States. J Nutr. 2009 Jun;139(6): 1228S-1235S.
Martin R, Barron JJ, Zacker C. Irritable bowel syndrome: toward a cost-effective management approach. Am J Manag Care. 2001 Jul;7(8 Suppl): S268-275.
Morcos A, Dinan T, Quigley EM. Irritable bowel syndrome: role of food in pathogenesis and management. J Dig Dis. 2009 Nov;10(4): 237-246.
Moshfegh AJ, Friday JE, Goldman JP, Ahuja JK. Presence of inulin and oligofructose in the diets of Americans. J Nutr. 1999 Jul;129(7 Suppl): 1407S-1411S.
Nelis GF, Vermeeren MA, Jansen W. Role of fructose-sorbitol malabsorption in the irritable bowel syndrome. Gastroenterology. 1990 Oct;99(4): 1016-1020.
Olesen M, Gudmand-Hoyer E. Efficacy, safety, and tolerability of fructooligosaccharides in the treatment of irritable bowel syndrome. Am J Clin Nutr. 2000 Dec;72(6): 1570-1575.
Ong D, Mitchell S, Barrett J, Shepherd S, Irving P, Biesiekierski J, Smith S, Gibson P, Muir J. Manipulation of dietary short chain carbohydrates alters the pattern of gas production and genesis of symptoms in irritable bowel syndrome. J Gastroenterol Hepatol. 2010 Aug;25(8): 1366-1373.
Ostgaard H, Hausken T, Gundersen D, El-Salhy M. Diet and effects of diet management on quality of life and symptoms in patients with irritable bowel syndrome. Mol Med Rep. 2012 Jun;5(6): 1382-1390.
Park YK, Yetley EA. Intakes and food sources of fructose in the United States. Am J Clin Nutr. 1993 Nov;58(5 Suppl): 737S-747S.
Pedersen A, Sandstrom B, Van Amelsvoort JM. The effect of ingestion of inulin on blood lipids and gastrointestinal symptoms in healthy females. Br J Nutr. 1997 Aug;78(2): 215-222.
Quigley E, Fried M, Gwee KA, Olano C, Guarner F, Khalif I, Hungin P, Lindberg G, Abbas Z, Bustos- Fernandez L, Mearin F, Bhatia SJ, Hu PJ, Schmulson M, Krabshuis JH, Le Mair AW. Irritable bowel syndrome: a global perspective. 2009. W. G. O. G. Guideline.
Ragnarsson G, Bodemar G. Pain is temporally related to eating but not to defaecation in the irritable bowel syndrome (IBS). Patients’ description of diarrhea, constipation and symptom variation during a prospective 6-week study. Eur J Gastroenterol Hepatol. 1998 May;10(5): 415-421.
Riby JE, Fujisawa T, Kretchmer N. Fructose absorption. Am J Clin Nutr. 1993 Nov;58(5): 748S-753S.
Rumessen JJ, Gudmand-Hoyer E. Fructans of chicory: intestinal transport and fermentation of different chain lengths and relation to fructose and sorbitol malabsorption. Am J Clin Nutr. 1998 Aug;68(2): 357-364.
Sachdeva S, Rawat AK, Reddy RS, Puri AS. Small intestinal bacterial overgrowth (SIBO) in irritable bowel syndrome: frequency and predictors. J Gastroenterol Hepatol. 2011 Apr;26 Suppl 3: 135-138.
Saito YA, Petersen GM, Locke GR, Talley NJ. The genetics of irritable bowel syndrome. Clin Gastroenterol Hepatol. 2005 Nov;3(11): 1057- 1065.
Shepherd S J, Gibson PR. Fructose malabsorption and symptoms of irritable bowel syndrome: guidelines for effective dietary management. J Am Diet Assoc. 2006 Oct;106(10): 1631-1639.
Shepherd SJ, Parker FC, Muir JG, Gibson PR. Dietary triggers of abdominal symptoms in patients with irritable bowel syndrome: randomized placebo-controlled evidence. Clin Gastroenterol Hepatol. 2008 Jul;6(7): 765-771.
Simren M, Barbara G, Flint HJ, Spiegel BM, Spiller RC, Vanner S, Verdu EF, Whorwell PJ, Zoetendal EG. Intestinal microbiota in functional bowel disorders: a Rome foundation report. Gut. 2013 Jan;62(1): 159-176.
Simren M, Mansson A, Langkilde AM, Svedlund J, Abrahamsson H, Bengtsson U, Bjornsson ES. Food-related gastrointestinal symptoms in the irritable bowel syndrome. Digestion. 2001;63(2): 108-115.
Spiller R, Aziz Q, Creed F, Emmanuel A, Houghton L, Hungin P, Jones R, Kumar D, Rubin G, Trudgill N, Whorwell P. Guidelines on the irritable bowel syndrome: mechanisms and practical management. Gut. 2007 Dec;56(12): 1770-1798.
Staudacher HM, Whelan K, Irving PM, Lomer MC. Comparison of symptom response following advice for a diet low in fermentable carbohydrates (FODMAPs) versus standard dietary advice in patients with irritable bowel syndrome. J Hum Nutr Diet. 2011 Oct;24(5): 487-495.
Stone-Dorshow T, Levitt MD. Gaseous response to ingestion of a poorly absorbed fructo-oligosaccharide sweetener. Am J Clin Nutr. 1987 Jul;46(1): 61-65.
Swagerty DL, Jr., Walling AD, Klein RM. Lactose intolerance. Am Fam Physician. 2002 May;65(9): 1845-1850.
Symons P, Jones MP, Kellow JE. Symptom provocation in irritable bowel syndrome. Effects of differing doses of fructose-sorbitol. Scand J Gastroenterol. 1992 Nov;27(11): 940-944.
Truswell AS, Seach JM, Thorburn AW. Incomplete absorption of pure fructose in healthy subjects and the facilitating effect of glucose. Am J Clin Nutr. 1988 Dec;48(6): 1424-1430.
van Loo J, Coussement P, de Leenheer L, Hoebregs H, Smits G. On the presence of inulin and oligofructose as natural ingredients in the western diet. Crit Rev Food Sci Nutr. 1995 Nov;35(6): 525-552.
Vazquez-Roque MI, Camilleri M, Smyrk T, Murray JA, Marietta E, O’Neill J, Carlson P, Lamsam J, Janzow D, Eckert D, Burton D, Zinsmeister AR. A controlled trial of gluten-free diet in patients with irritable bowel syndrome-diarrhea: effects on bowel frequency and intestinal function. Gastroenterology. 2013 May;144(5): 903-911 e903.
Ventura EE, Davis JN, Goran MI. Sugar content of popular sweetened beverages based on objective laboratory analysis: focus on fructose content. Obesity (Silver Spring). 2011 Apr;19(4): 868-874.
Vernia P, Marinaro V, Argnani F, Di Camillo M, Caprilli R. Selfreported milk intolerance in irritable bowel syndrome: what should we believe? Clin Nutr. 2004 Oct;23(5): 996-1000.