Estrogen metabolism
Advances in prediction of disease risk
Since the late 1990’s researchers have been using immunoassays to measure certain estrogen metabolites (2- and 16-hydroxyestrogens) in urine, in an attempt to gauge future risk of breast and prostate cancer, and many practitioners have used these immunoassay measurements in their practices for the past decade. A 2011 meta-analysis examined the body of literature on this topic and questions its validity. This article reviews the conclusions of the meta-analysis and briefly discusses future directions for research, using the newer, LCMSMS technology.
In the last several decades there has been increased recognition that elevated levels of estrogens are causally related to breast cancer (Ziegler 2010). This has led to increased interest in how estrogens are broken down in the body including how various nutritional deficiencies and genetic tendencies relevant to cancer may affect the pattern of urine estrogen metabolites.
Our understanding of estrogen metabolism has been largely shaped by the measurement technologies available. Past measurement techniques have included immunoassays (RIA and ELISA) as well as gas chromato graphic-mass spectrometric (GCMS) methods (Stanczyk 2007). The latest methodology uses liquid chromatography-tandem mass spectrometry (LCMSMS), which is said to provide improved accuracy and specificity (Falk 2008). Certain long-held ideas about estrogen metabolism now need to be revisited in light of improvements in our ability to measure estrogen metabolites.
This review summarizes what we know about the interpretation of urine estrogen metabolite measurements in light of the most recent research and technological developments. In short, it appears that the traditional urine estrogen metabolite ratio measured by ELISA is of less utility for gauging risk of breast cancer than previously thought. It is also apparent that LCMSMS measurements of the urine estrogen metabolites cannot be interpreted in the same way as the older ELISA data. There is increased interest in lesser-studied metabolites such as 4-hydroxyestrone, and 2-methoxyestrone for assessment of risk of estrogen-sensitive cancers, and the development of newer methodologies is sure to usher in further advances in estrogen metabolism research.
2:16 ratio Around 1997, the Estramet™ ELISA estrogen metabolite kit was introduced as a means to measure the ratio of 2-hydroxylated estrogens to 16-hydroxylated estrone. This ratio is often referred to as the “2/16 ratio” or “Estrogen Metabolism Ratio (EMR)”. Based on literature suggesting that 16-hydroxyestrone was carcinogenic and that 2-hydroxyestrogens were protective or at least cancer-neutral, the ratio was deemed to be relevant for breast cancer risk assessment (Lord 2008). A lower ratio (lower than normal 2-hydroxyestrogens) was thus thought to reflect an excess of “bad” estrone (16OHE1) relative to the good/benign estrogens. Numerous therapies have been shown to increase this ratio, mostly by upregulating the enzymes that make 2-hydroxyestrogens (Lord 2002). The rationale for increasing the EMR was to decrease future risk of breast cancer, although this has never been prospectively or retrospectively studied.
Like many immunoassays, the Estramet™ kit lacks specificity, which is evidenced by the fact that the antibody ostensibly directed toward 2-hydroxyestrone cross-reacts with other 2-hydroxylated estrogens (IBL Estramet™ 2008). In other words, two individuals may have the same value for total 2-hydroxyestrogens, but the proportional values of 2-hydroxyestrone (2OHE1), 2-hydroxyestradiol (2OHE2) and 2-hydroxyestriol (2OHE3) may be quite different for each. This makes the interpretation of data generated by the ELISA kit somewhat problematic.
When the Estramet™ kit was introduced in the late 1990’s, it was used in several published prospective and population-based case control studies on the risk of breast cancer. Based on these studies, practitioners understood that an Estramet™ ratio of less than approximately two was associated with increased breast cancer risk in both pre- and postmenopausal women not currently using estrogen therapy (Kabat 1997, Meilahn 1998, Muti 2000). The increased risk of breast cancer comparing the highest to lowest quantiles of the EMR was estimated to be between 15 and 30%, with weak statistical significance (Obi 2011).
More recent literature suggests a need to reevaluate these assumptions. A 2011 meta-analysis by Obi et al reviewed all the literature on the EMR specifically for non-estrogen users and concluded: “For the highest compared with the lowest quantile of urinary EMR, non-significant associations suggested at best a weak protective effect in premenopausal but not in postmenopausal breast cancer (range of odds ratios: 0.50–0.75 for premenopausal and 0.71–1.31 for postmenopausal)” (Obi 2011). In other words, there is no evidence that a higher EMR protects postmenopausal women from breast cancer, and there is weak evidence of a protective effect in premenopausal women. For each of the studies included in Obi’s metaanalysis, a risk reduction or risk increase was calculated by comparing the highest EMRs to the lowest EMRs. Only one of these studies, conducted in China, showed a significant decrease in breast cancer risk. Other studies looking at North American or European populations produced results that clustered around a relative risk of 1 – an indication of no effect on breast cancer risk (Obi 2011). Hence, the notion that the EMR (measured by immunoassay) is associated with breast cancer risk is not on a robust statistical foundation.
The EMR is on even shakier ground when viewed through the lens of estrogensupplementing women. A prospective casecontrol analysis authored by Wellejus (2005) looked at the predictive value of the EMR (as measured by Estramet™) for breast cancer risk in postmenopausal women using estradiolbased HRT. Unlike the no-effect or weakly protective effect of the higher EMR on breast cancer risk in non-estrogen users, Wellejus found that higher EMRs were associated with an increased risk of estrogen receptor positive breast cancer in women supplementing with estradiol-based hormone therapy. The authors found that this increased risk was tied to increased levels of 2-hydroxyestrogens and was independent of 16-hydroxyestrone (16OHE1); they commented that presentation of the metabolites as a ratio is probably misleading in postmenopausal women supplementing with estradiol (Wellejus 2005).
Assuming that there is value in knowing the EMR, should we try to use the urinary levels of specific 2-hydroxylated estrogen metabolites (2OHE1 and 2OHE2) more accurately measured via LCMSMS to calculate an approximation of the immunoassay method EMR? If so, how should laboratories determine the correct threshold?
One laboratory addresses this issue by measuring estrogen metabolite levels both ways: via LCMSMS and via immunoassay, reporting the individual LCMSMS numbers for hydroxyestrones and hydroxyestradiol and reporting the EMR based on immunoassay numbers (Genova Diagnostics references I 2013, Genova Diagnostics II 2013). Another laboratory uses LCMSMS to measure all metabolites, and derives an approximation of the EMR from the following: (2OHE2 + 2OHE1)/16OHE1. The threshold for this LCMSMS ratio was chosen to divide the sample population in the same fashion as did the immunoassay threshold ratio (Metametrix 2013). Ideally, the two thresholds would numerically match, but in practice the LCMSMS threshold is higher. This reflects the fact that the two methodologies are not measuring exactly the same things. In order to properly resolve the issue, new prospective studies would have to be performed using LCMSMS methodology.
An important consideration when working with ratios is their potential to shift focus away from the component numbers. For example, elevated 2-hydroxylated estrogen metabolites are a problem regardless of their level in relation to 16OHE1 (as noted by Wellejus). Conversely if all estrogen metabolite levels are very low, is an abnormal ratio really relevant? Likely not.
EMR in Males
There are several case-control retrospective studies looking at a possible connection between prostate cancer and the EMR (Barba 2009). In general, these studies suggest a weak association between a low EMR and prostate cancer risk. Muti, for example, found that men in the highest tertile for EMR had an 39% lower risk of prostate cancer (OR of 0.61) compared to the lowest tertile, but the confidence interval was wide and crossed 1 (no effect) (Muti 2002). As is the case for women and breast cancer, there are no controlled trials that show a higher EMR protects against prostate cancer, nor any that show that a therapeutic increase in the EMR will lower the risk of prostate cancer. In short, given the current state of research, it appears the EMR is no more valuable in males than it is in females.
In summary, it is this author’s opinion that there is minimal value in reporting the EMR or an approximation thereof in either women or men. There is likely more value in measuring individual metabolite levels. For example, when estrogens are being supplemented (particularly oral estradiol), elevation of “2-hydroxyestrogens” appears to be associated with an increased risk of breast cancer (Wellejus 2005). This leads naturally to the question of whether there is value in examining other estrogen metabolites, or in examining metabolites in different ways.
Hydroxyestrone vs Hydroxyestradiol None of the previously discussed immunoassay studies address the issue of the relative proportions of 2-hydroxyestrone and 2-hydroxyestradiol metabolites. This may be of particular importance when 2-hydroxyestrogens are high. Using an immunoassay like the Estramet™, it is impossible to know if elevated 2-hydroxyestrogens are a result of elevated 2OHE1, 2OHE2 or both because the individual metabolites are indistinguishable to the antibodies. It is therefore worth asking the question: are the relative amounts of each type of estrogen important in the overall total?
To answer that question, it is important to know the following: the various estrogens can exist in either estrone or estradiol form. The enzyme that converts estradiol to its estrone form is 17-hydroxysteroid dehydrogenase Type II. Estrogen pairs that regularly undergo conversion include estrone/estradiol, 2-hydroxyestrone/2- hydroxyestradiol, 4-hydroxyestrone/4-hydroxyestradiol and others (Kitawaki 2000).
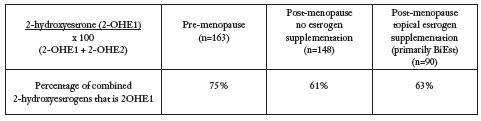
Rocky Mountain Analytical has reviewed the partitioning of 2-hydroxyestrogens measured via LCMSMS in first morning urine in a population of women (including women with both recent and remote diagnoses of breast cancer. The data below are presented without regard to breast cancer status. The results are summarized below.
The estrone metabolite appears to be favoured over the estradiol metabolite as the ratio of 2OHE1 to 2OHE2 exceeds 50% across all groups. The lower percentage of 2OHE1 in post-menopause relative to pre-menopause probably reflects differential expression of 17-hydroxysteroid dehydrogenase Type II. Progesterone is known to induce this enzyme (Kitawaki 2000), which means the higher proportion of 2OHE1 relative to 2OHE2 in pre-menopause is likely a consequence of higher progesterone levels found in premenopausal women.
Research published by Huang in late 2011 examined 16 different estrogen metabolites in the urine of postmenopausal women with breast cancer versus healthy controls. The breast cancer patients were found to have higher levels of both 2- and 4-hydroxyestradiol compared to healthy controls. The proportions between estrones and estradiols could only be estimated, as their data did not report 2- and 4-hydroxyestrones separately. Their research does however support the notion that although estrogens are supposed to be able to freely interconvert between the estrone and estradiol forms, the equilibria lie more toward the estradiol side in breast cancer patients (Huang 2012).
The point of the preceding discussion is that it is probably time to move away from some of the older concepts about estrogen metabolism and breast cancer, and start mining the specific (and copious) data provided by LCMSMS technology.
Methoxyestrogens
Further metabolism of hydroxyestrogens involves conversion of a hydroxyl (-OH) group to a methoxy group (-OCH3). Hence there is a family of methoxyestrogens including 2-methoxyestradiol, 2-methoxyestrone, 4-methoxyestradiol and 4-methoxyestrone, which mirror the hydroxyestrogens (Obi 2011).
There is some literature indicating that methoxyestrogens may be relevant for assessing risk of breast cancer. For example, the study by Huang, mentioned earlier noted lower levels of 2-methoxyestradiol (2-MeOE2) in breast cancer patients compared to controls (Huang 2012). In particular 2-MeOE2, the downstream metabolite of 2-hydroxyestradiol, is thought to mitigate against breast cancer by a variety of mechanisms including anti-angiogenesis and cell cycle regulation (Mueck 2010). This molecule is the focus of active research as a potential treatment for breast cancer.
Huang et al speculated in their paper: “Interestingly, 2-MeOE2 levels, with a p-value of 0.038, were significantly reduced in breast cancer cases. It is speculated that methylation of catechol estrogens might prevent reactive quinine formation as well as weaken binding to the estrogen receptor, both of which should be beneficial for decreased breast cancer risk. Because methylation plays an important role in the protection against rapid tumor growth, 2-MeOE2 could be presumed a potential anticancer biomarker for breast cancer” (Huang 2012).
Conversion of hydroxyestrogen to methoxyestrogen is a transmethylation reaction requiring an adequate supply of methyl donors and magnesium (enzyme cofactor) as well as sufficient catechol orthomethyltransferase (COMT) enzyme activity (Cavalieri 2011). Reduced levels of methoxyestrogens relative to their parent hydroxyestrogens may therefore reflect nutritional factors (insufficient levels of folic acid, B12, magnesium, betaine, SAMe, and/or MSM) plus genetic factors (homo- or heterozygosity for hypofunctioning COMT alleles) (Cavalieri 2011). Hypofunctioning mutations of COMT have been noted in various populations of women with breast cancer (Yager 2000). To date, no prospective trials looking at the predictive value of low levels of 2-methoxyestrogens in relation to breast cancer have been reported.
Once again from the data presented by Huang, the ratio of methoxyestrogen/parent hydroxyestrogen was calculated for postmenopausal breast cancer patients versus healthy postmenopausal controls. In general, the ratios became smaller (closer to zero) for breast cancer patients compared to controls, possibly indicating that there was less methoxylation of parent hydroxyestrogens in breast cancer patients, and supporting the notion that it may be worthwhile to measure and track these various parameters (Huang 2012).
4-Hydroxyestrone
At the time that 16-hydroxyestrone was being put forth as a “bad estrogen”, 4-hydroxyestrone was also emerging as an important metabolite in relation to breast cancer. On balance, evidence is fairly compelling to support a role for 4-hydroxyestrone in breast cancer causation. An extensive monograph on this topic was published in 2000 (Jefcoate 2000). Ercole Cavalieri, a principal researcher in this field, has also published an excellent review (Cavalieri 2002).
The proposed carcinogenic action of 4OHE1 is as follows: after conversion to a quinone form, 4-hydroxyestrone may irreversibly bind to DNA, resulting in removal of purine bases (Cavalieri-1997, 2002). Depurination of oncogenic stretches of DNA may be a very early event in the genesis of breast cancer (Cavalieri 2000).
By cycling back and forth between the semiquinone and quinone forms, 4-hydroxyestrone also generates free radicals, with resultant DNA damage and lipid peroxidation (Davis 1997, Cavalieri 1997).
Gaikwad et al demonstrated that women with untreated breast cancer had the highest levels of purine adducts with 4-hydroxyestrone compared to healthy controls and women at high risk of breast cancer. Conversely, the patients with cancer had the lowest levels of thiol conjugates (including glutathione conjugates) of 4-hydroxyestrone (Gaikwad 2009). Conjugation with glutathione and other thiol-containing molecules prevents depurinating adduct formation (Cavalieri 2011). Low levels of thiol conjugates would imply less protection. Breast cancer patients also had the lowest levels of 4-methoxyestrone, which is another mechanism whereby 4-hydroxyestrone is “detoxified”. However, there is still some controversy regarding the utility of urinary 4OHE1 (as conjugate) levels for assessing breast cancer risk. Gaikwad presented data indicating lower levels of 4-hydroxyestrone in breast cancer patients compared to controls. Rocky Mountain Analytical data shows the opposite, with highest levels of 4-hydroxyestrone appearing in breast cancer patients. This apparent conflict may be a result of different testing methodologies. In any case, the mass balance of estrogen in the 4-hydroxyestrone ‘branch’ of the estrogen metabolism tree appears to be an exciting avenue for future research.
Closing Remarks
The relationship between breast cancer and estrogen metabolites continues to be an active area of research. Emphasis needs to shift away from the 2-16 ratio and toward estrogen metabolite profiles which are more closely linked to breast cancer. Further research may also be directed towards analytes that inform on DNA damage and glutathione deficiency. This is a fascinating area of Women’s Health in which analysis of urine estrogen metabolites via LCMSMS has much to offer.
References
Barba M, Yang L, Schünemann HJ, Sperati F, Grioni S, Stranges S, Westerlind K, Blandino G, Gallucci M, Lauria R, Malorni L, Muti P. Urinary estrogen metabolites and prostate cancer: a case-control study and meta-analysis. J Exp Clin Cancer Res 2009;28:135.
Cavalieri EL, Stack DE, Devanesan PD, Todorovic R, Dwivedy I, Higginbotham S, Johansson SL, Patil KD, Gross ML, Gooden JK, Ramanathan R, Cerny RL, Rogan E. Molecular origin of cancercatecholestrogen 34-quinones as endogenous tumour initiators. Proc Natl Acad Sci. 1997;94:10937-42
Cavalieri EL, Frenkel K, Liehr JG, Rogan E, Roy D. Estrogens as endogenous genotoxic agents–DNA adducts and mutations. J Natl Cancer Inst Monogr. 2000;27:75-93
Cavalieri E, Rogan E, Chakravarti D. Initiation of cancer and other diseases by catechol ortho-quinones: a unifying mechanism. Cell Molec Life Sci 2002;59:665-681.
Cavalieri E, Rogan E. Unbalanced metabolism of endogenous estrogens in the etiology and prevention of human cancer. J Steroid Biochem Mol Biol. 2011; 125:169–180
Davis DL, Telang NT, Osborne MP, Bradlow HL. Medical Hypothesis: Bifunctional Genetic-Hormonal Pathways to Breast Cancer. Environmental Health Perspect. 1997;105(Suppl 3):571-76.
Falk RT, Xu S, Keefer L, Veestra TD, Ziegler RG. A liquid chromatography-mass spectrometry method for the simultaneous measurement of 15 urinary estrogens and estrogen metabolites: assay reproducibility and interindividual variability. Cancer Epidemiol Biomarkers PRev. Dec 2008;17(12):3411-18
Faupel-Badger JM, Fuhrman BJ, Xu X, Falk RT, Keefer LK, Veenstra TD, Hoover RN, Ziegler RG. Comparison of liquid chromatography-tandem mass spectrometry, RIA, and ELISA methods for measurement of urinary estrogens. 2010. Jan;19(1):292-300
Gaikwad NW, Yang L, Pruthi S, Ingle JN, Sandhu N, Rogan EG, Cavalieri EL. Urine biomarkers of risk in the molecular etiology of breast cancer. Breast Cancer (Auckl) 2009 Jan 6;3:1-8.
Genova Diagnostics I – Essential Estrogens Sample Report. URL : http://www.gdx.net/core/sample-reports/Essential-Estrogens-FMVSample- Report.pdf Accessed January 8, 2013
Genova Diagnostics II-Urine Estrogen Metabolism Assessment- One Page Description. URL: http://www.gdx.net/core/one-pagetest- descriptions/Estrogen-Metabolism-Assess-Test-Description.pdf Accessed January 9,2013.
Huang J, Sun J, Chen Y, Song Y, Dong L, Zhan Q, Zhang R, Abliz Z. Analysis of multiplex endogenous estrogen metabolites in human urine using ultra-fast liquid chromatography-tandem mass spectrometry: A case study for breast cancer. Anal Chim Acta 2012;711:60-68. Epub 2011 Nov 7.
IBL Estramet™ 2/16 ELISA Instructions for Use. 2008-10- 01. URL: http://www.ibl-international.com/magento/media/ catalog/product/I/A/IA52011_IFU_en_Estramet_2-16_ ELISA_2006-23-01_int.pdf Accessed January 9, 2013.
Jefcoate CR, Liehr JG, Santen RJ, Sutter, TR, Yager JD, Yue W, Santner SJ, Tekmal R, Demers L, Pauley R, Naftolin F, Mor G, Berstein L. Chapter 5: Tissue Specific Synthesis and Oxidative Metabolism of Estrogens. JNCI Monographs, No. 27, 95-112, 2000.
Kabat GC, Chang CJ, Sparano JA Urinary estrogen metabolites and breast cancer : a case-control study. Cancer Epidemiol Biomarkers Prev. 1997;6(7):505-509
Kitawaki J, Koshiba H, Ishihara H, Kusuki I, Tsukamoto K, Honjo H. Progesterone induction of 17beta-hydroxysteroid dehydrogenase type 2 during the secretory phase occurs in the endometrium of estrogen-dependent benign diseases but not in normal endometrium. J Clin Endocrinol Metab. 2000 Sep;85(9):3292-6.
Lord RS, Bralley JA eds. 2008. Chapter 10, Hormones. Laboratory Evaluations for Integrative and Functional Medicine. Metametrix Institute, Duluth, GA 2008:569-72
Lord RS, Bongiovanni B, Bralley JA. Estrogen Metabolism and the Diet-Cancer Connection: Rationale for Assessing the Ratio of Urinary Hydroxylated Estrogen Metabolites. Alt Med Review. 2002;7(2):112-29.
Meilahn EN, de Stavola B, Allen DS, Fentiman I, Bradlow HL, Sepkovic DW, Kuller LH. Do urinary oestrogen metabolites predict breast cancer? Guernsey III cohort follow-up. Br J Cancer. 1998;78(9):1250-55
Metametrix – Estronex Sample Report. URL: http://www. metametrix.com/files/test-menu/sample-reports/Estronex-SR.pdf Accessed January 8, 2013
Mueck AO, Seeger H. 2-Methoxyestradiol–biology and mechanism of action. Steroids 2010;75:625-631. Epub 2010 Mar 7.
Muti P, Bradlow HL, Micheli A et al. Estrogen metabolism and risk of breast cancer : a prospective study of the 2:16 alpha-hydroxyestrone ratio in premenopausal and postmenopausal women. Epidemiology. 2000;11(6):635-40
Muti P, Westerlind K, Wu T, Grimaldi T, De Berry J 3rd, Schünemann H, Freudenheim JL, Hill H, Carruba G, Bradlow L. Urinary estrogen metabolites and prostate cancer: a case-control study in the United States. Cancer Causes Control 2002;13:947-955.
Obi N, Vrieling A, Heinz J, Chang-Claude. Estrogen metabolite ratio: Is the 2-hydroxyestrone to 16α-hydroxyestrone ratio predictive for breast cancer? J. Int J Womens Health 2011;3:37-51.
Stanczyk F, Lee JS, Santen RJ. Standardization of Steroid Hormone Assays: Why, How and When? Cancer Epidemiol Biomarkers Prev. 2007;16:1713-19.
Wellejus A, Olsen A, Tjonneland A, Thomsen BL, Overvad K, Loft S. Urinary hydroxyestrogens and breast cancer risk among postmenopausal women: a prospective study. Cancer Epidemiol Biomarkers Prev. 2005 Sep;14(9):2137-42.
Yager JD. Endogenous estrogens as carcinogens through metabolic activation. J Natl Cancer Inst Monogr. 2000;27:67-73 Ziegler RG, Faupel-Badger JM, Sue LY, Falk RT, Boyd-Morin J, Henderson MK, Hoover RN, Veenstra TD, Keefer LK, Xu X. A new approach to measuring estrogen exposure and metabolism in epidemiologic studies. J Steroid Biochem Mol Biol 2010;121:538-545.