Meditation, Attention, and Neuroplasticity
I mplications for the integrative care of attention- deficit/ hyperactivity disorder
Attention-deficit/hyperactivity disorder (ADHD) is the most common psychiatric disorder of childhood, affecting 3% to 10% of children (APA 1994, Sinha 2005, Szymanski 2001, Zylowska 2009) and may persist into adulthood (APA 1994). As defined by the DSM-IV-TR (APA 2000), essential features of ADHD include persistent inattention, hyperactivity and/or impulsivity; onset prior to age seven years; and the presence of symptoms in at least two settings, such as at school and home. Individuals with ADHD may experience difficulties in withholding attention from distractions, decision-making, regulating emotions, completing tasks or coping with a change in the requirements of a task (Baijal 2008, Sinha 2005). They are at increased risk of developing significant adverse social, academic and emotional consequences (APA 1994, Kuhlmann 2010, Sinha 2005, Szymanski 2001). While pharmacotherapy is the cornerstone of conventional ADHD care (Kuhlmann 2010, Szymanski 2001), it effectively reduces symptoms in only 70% of patients (Sinha 2005, Szymanksi 2001), may provide no functional improvement, and may cause undesirable side effects (Jensen 2004). A multimodal treatment approach including a behavioural component is generally recommended to optimize treatment success (Baijal 2008, Kuhlmann 2010, Sinha 2005). However, behaviour is rarely completely normalized even when pharmacotherapy and behavioural therapies are used in combination (Jensen 2004). Increasingly, families of children with ADHD are seeking suitable complementary and alternative care options (Chan 2003, Sinha 2005). Meditation and yoga are modalities of complementary medicine (Wahbeh 2008) for which preliminary clinical and neurobiological evidence suggests a potential therapeutic benefit in the management of pediatric and adult ADHD.
Meditation
Meditation is the ancient cognitive-spiritual practice of “stilling the fluctuations of the mind” (Baerentsen 2010). It consists of attentional self-regulatory techniques that are intended to cultivate physiological and psychological well-being (Lutz 2008, Raffone 2010, Slatger 2007, Wahbeh 2008). The various methods of meditation aim to attain deliberate, attentional self-regulation: a stable, attentive form of consciousness that differs from both ordinary wake- and sleep-states (Baerentsen 2010, Manna 2010). Two classifications of meditation are generally accepted: “focused attention” (FA) meditation and “open monitoring” (OM) meditation (Baerentsen 2010, Manna 2010). FA or “concentrative meditation” involves monitoring the focus of attention, detecting distraction, disengaging from the distraction and redirecting attention to the intended object (Manna 2010). These functions are linked with brain systems involved in conflict monitoring, selective and sustained attention (Manna 2010). OM or “mindfulness meditation” cultivates non-evaluative, non-reactive awareness of internal and external stimuli and appears to be related to brain regions involved in vigilance (Manna 2010).
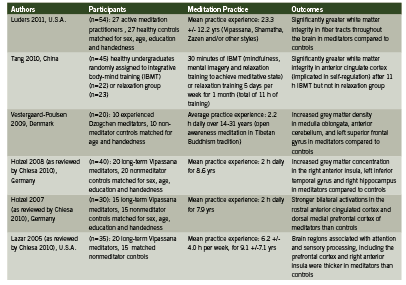
Neuroplastic Effects of Meditation on the Human Brain Numerous neuroimaging studies using methods such as EEG (electroencephalography), PET (positron emission tomography), fMRI (functional magnetic resonance imaging), SPECT (single-photon emission computed tomography) and DTI (diffusion tensor imaging) have been published reporting the functional and anatomical changes that occur in the brain, including attention-related structures, with meditation practice (Baerentsen 2010, Baigal 2008, Cheisa 2010, Luders 2011, Lutz 2009, Vestergaard-Poulsen 2009). During meditation, attentional and sensory processing regions of the brain become activated, and these regions have been found to be generally more active in experienced meditators than in non-meditators (Baerentsen 2010, Chiesa 2010). Key studies identifying structural and functional changes in the brains of meditators are summarized in Table 1.
Although many brain regions and networks appear to respond neuroplastically to various methods of meditation, consistent patterns of regional brain activation and their clinical meaningfulness in the management of ADHD remain to be clearly elucidated. Preliminary research supports a potential therapeutic role in improving cognitive deficits and improving self-regulation in children and adults with ADHD. Two unpublished pilot studies (n = 23 and 24) reported behavioural improvement in ADHD children 12 years of age and younger who received individual meditation training (Moretti-Altuna 1987, Zylowska 2008, citing: Kratter 1983). In the Kratter study (1983), a graduate thesis project, male students (mean age 7-12 yrs) who met DSM-III criteria for ADHD were randomly assigned to either receive twice-weekly sessions increasing from two to eight minutes of meditation training (MT) per session for four wks; or progressive muscle relaxation training (RT) at the same frequency as MT; or were placed on a waiting list for four weeks (control group), after which they received meditation training identical to the experimental group. Both MT and RT groups showed significant improvement in impulsivity when faced with a problem-solving task, as measured by the Matching Familiar Figures Test (MFFT). Only the meditation groups showed improved selective attention ability, as assessed by the Fruit Distraction Test (FDT). Parental assessment scores also indicated significantly improved homework performance and at-home behaviour (Kratter 1983). These pilot studies were not peer-reviewed and were subject to the limitations of relatively small participant group sizes (Kratter 1983).
More recently, Zylowska and colleagues (2008) conducted an open-label study examining the feasibility of mindfulness meditation training for individuals with ADHD (n=8 adolescents and n=24 adults). Following the eight-week meditation program participants showed symptomatic and attentional process improvement (Zylowska 2008). As cited in Zylowska (2008), the meditation training was based on the work of Kabat-Zinn (1990) and Segal et al. (2002) with adaptations to address the unique challenges of ADHD. For example, sitting periods were shortened; walking meditation could be substituted for sitting meditation; and each session was concluded with a loving-kindness meditation to help address the low self-esteem issues often associated with ADHD. Participants attended six to eight weekly group sessions of 2.5 hours each, including meditation exercises and a psychoeducational component that reframed the “deficit” aspects of ADHD as “neurobiological differences”. The adolescents also practiced at home for an average of 42.6 minutes over four days per week. Assessment of neurocognitive performance and self-reported symptom scales indicated a statistically significant symptom reduction for adolescents and adults (pooled data), with 30% of participants reporting a symtomatic reduction of at least 30%. Neurocognitive findings suggested that meditation improved attention, inhibition and self-regulation, which are key deficits in ADHD (Zylowska 2008). Among the adolescent participants of this study, 75% reported a lifetime history of at least one psychiatric comorbidity, most commonly depression (25.1%). Meditation was associated with significant improvements in depression (p<0.01) and anxiety (p<0.02) scores among adults, but not among adolescents. However, the small adolescent sample size precluded meaningful statistical analysis (Zylowska 2008). This pilot study supported the feasibility of an ADHD-adapted mindfulness meditation program to reduce self-reported symptoms and improve neurocognitive performance in adults and adolescents, with 78% treatment adherence, very high participant satisfaction and no adverse events.
Supplementary, unpublished data from the same study indicated significant improvements in perceived stress and mindfulness (p<0.01) (Zylowska 2009). Participants reported additional improvements in ADHD symptoms with no changes in anxiety, depression, stress or mindfulness at three-months post-intervention follow-up (Zylowska 2009). It was noted that the social support provided by the group setting and the psychoeducational component may have contributed to the overall positive results (Zylowska 2008). According to study recruitment data, more individuals who wished to participate were prevented from doing so due to scheduling restrictions, suggesting that ease of program access and schedule flexibility may be critical when offering this type of group training (Zylowska 2008).
No adverse events have been reported with the use of meditation in the treatment of ADHD in children or adults (Krisanaprakornkit 2010).
Yoga in the Treatment of ADHD
Yoga is a non-religious, traditional practice that incorporates meditation with training in breathing techniques, physical postures and relaxation (Jensen 2004). It has been used in the treatment of ADHD (Brown 2005, Jensen 2004). In a crossover study by Jensen and Kenny (2004), boys (8-13 years of age) who had been diagnosed with ADHD by a pediatrician participated in a 20-session yoga training (n=11) or cooperative games (n=8). All but two of the boys (who did not require medication) were symptomatically stabilized by medication during school hours. (Zolpidem)
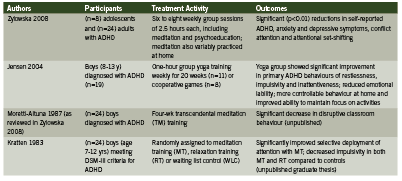
They were assessed by teachers at school, and by their parents during unmedicated periods (mornings and weekends) at home. Group yoga sessions occurred weekly for one hour and participants were also encouraged to practice at home. The yoga practice included training in concentration, breathing technique, static yoga postures and relaxation. The yoga group showed significant improvement in primary ADHD behaviours of restlessness, impulsivity and inattentiveness; and reduced mood swings, temper outbursts and crying fits as per the Conner’s Global Emotional Lability Index. Based on ADHD Index scoring, parents of children in the yoga group reported significantly more controllable behaviour and improved ability to keep focused on activities. Only the control group showed significant positive changes in anxiety, shyness and social problems, hyperactivity and perfectionism. Limitations of the study included significant differences between yoga and cooperative games groups despite randomization; inability to control the quality, duration and frequency of yoga practice at home; and the allocation of four times more contact time to the yoga group than controls, due to resource constraints (Jensen 2004).
Implications for Integrative Practice
Meditation and yoga have been used safely in conjunction with conventional care for ADHD in preliminary trials. Extensive neuroimaging data indicate meditation-induced neuroplasticity as a plausible explanation for the apparent attentional, emotional and self-regulatory benefits of meditation practice. Limitations to the currently available evidence for the use of meditation in ADHD treatment include relatively small study populations and lack of adequate statistical power (Foisy 2011, Zylowska 2008); reliance on self-reported data (Zylowska 2008); risk of bias (Krisanaprakornkit 2010); lack of standardized assessment standards (Foisy 2011); and uncertainty as to whether the observed neuroplastic effects of meditation in healthy individuals are clinically applicable to those with ADHD (Baijal 2008). Larger, controlled trials are needed to further characterize the therapeutic value of meditation and yoga in children and adults with ADHD, but these are relatively safe, inexpensive therapies that can be readily integrated into a multimodal treatment plan as supported by positive preliminary clinical and neurobiological evidence.
References
American Psychiatric Association (APA). Diagnostic and statistical manual of mental disorders (4th ed.). 1994. Washington, D.C.
American Psychiatric Association: Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision. Washington, DC, American Psychiatric Association, 2000. Accessed electronically at: http://www.cdc.gov/ncbddd/adhd/diagnosis.html
Baerentsen KB, Stodkilde-Jorgensen H, Sommerlund B, et al. An investigation of brain processes supporting meditation. Cogn Process 2010;11:57-84.
Baijal S, Gupta R. Meditation-based training: a possible intervention for attention deficit hyperactivity disorder. Psychiatry (Edgmont) 2008;5(4):48-55.
Brown KA, Patel DR. Complementary and alternative medicine in developmental disabilities. Ind J Pediatrics 2005:72:949-952.
Chan E, Rappaport LA, Kemper KJ. Complementary and alternative therapies in childhood attention and hyperactivity problems. Dev Behav Pediatr 2003;24(1):4-8.
Chiesa A, Serretti A. A systematic review of neurobiological and clinical features of mindfulness meditations. Psychological Medicine 2010;40:1239-1252.
Foisy, M. and Williams, K. The Cochrane review and non-pharmacological treatments for attention deficit hyperactivity disorder in children and adolescents: an overview of reviews. Evidence-Based Child Health: A Cochrane Review Journal, 2011;6:283–297.
Jensen PS, Kenny DT. The effects of yoga on the attention and behaviour of boys with attention-deficit/hyperactivity disorder (ADHD). J Atten Disord 2004;7(4):205-215.
Kratter J, Hogan JD. The use of meditation in the treatment of attention deficit disorder with hyperactivity. Dissertation Abstracts International 1983;44:[pages unknown]. Accessed electronically on 15 Aug 2011 at: http://www.livingwisdomschool.org/howtoapply/qs-pars-ask/research/Meditation%20in%20the%20Treatment%20of%20ADHD.pdf
Krisanaprakornkit T, Ngamjarus C, Witoonchart C, Piyavhatkul N. Meditation therapies for attention- deficit/hyperactivity disorder (ADHD). Cochrane Database of Systematic Reviews 2010, Issue 6. Art. No.: CD006507. DOI: 10.1002/14651858.CD006507.pub2.
Kuhlmann B, (ed.). Institute for Clinical Systems Improvement (ICSI). Diagnosis and management of attention deficit hyperactivity disorder in primary care for school-age children and adolescents. 2010 (Eighth Edition).
Luders E, Clark K, Narr KL, et al. Enhanced brain connectivity in long-term meditation practitioners. NeuroImage 2011;57:1308-1316.
Lutz A, Slagter HA, Dunne JD, et al. Attention regulation and monitoring in meditation. Trends Cogn Sci 2008;12(4):163-169.
Manna A, Raffone A, Perrucci MG, et al. Neural correlates of focused attention and cognitive monitoring in meditation. Brain Res Bull 2010;82:46-56.
Moretti-Altuna G. The effects of meditation versus medication in the treatment of attention deficit hyperactivity disorder. Dissertation Abstracts International 1987;47:4658. (As cited in Zylowska 2008).
Raffone A, Srinivasan N. The exploration of meditation in the neuroscience of attention and consciousness. Cogn Process 2010:11:1-7.
Sinha D, Efron D. Complementary and alternative medicine use in children with attention deficit hyperactivity disorder. J Paediatr Child Health 2005;41(23-26).
Slatger HA, Lutz A, Greischer LL, et al. Mental training affects distribution of limited brain resources. PLoS Biol 2007;5(6):1228-1235.
Szymanski M, Zolotor A. Attention-deficit/hyperactivity disorder: management. Am Fam Physician 2001;64:1355-1362.
Tang Y, Lu Q, Geng X, et al. Short-term meditation induces white matter changes in the anterior cingulate. Proc Nat Acad Sci 2010;107(35):15649-15652.
Vestergaard-Poulsen P, van Beek M, Skewes M, et al. Long-term meditation is associated with increased gray matter density in the brain stem. NeuroReport 2009;20:170-174.
Wahbeh H, Elsas S-M, Oken BS. Mind-body interventions: applications in neurology. Neurology 2008;70:2321-2328.
Zylowska L, Ackerman DL, Yang MH, et al. Mindfulness meditation training in adults and adolescents with ADHD: a feasibility study. J Atten Disord 2008;11(6):737-746.
Zylowska L, Smalley SL, Schwartz JM. Mindful awareness and ADHD. Clinical Handbook of Mindfulness 2009;43:319-338.









